Stopping your medication because of side effects is one of the most common mistakes people make - and it’s often unnecessary. You might feel dizzy after taking your blood pressure pill, get nauseous from your antidepressant, or notice dry mouth from your diabetes drug. It’s tempting to skip a dose or quit altogether. But before you do, there’s a better way: talk to your provider without quitting. Many side effects aren’t deal-breakers. They’re temporary, manageable, or even signs the drug is working. The key is knowing how to communicate them clearly - and what to say next.
Why You Shouldn’t Just Quit
About half of all people stop taking prescribed medications within the first year. Side effects are the top reason. But here’s the catch: many of those side effects fade. According to the British Heart Foundation, 68% of common drug side effects go away on their own within 7 to 14 days as your body adjusts. That means what feels unbearable today might be barely noticeable in two weeks. Quitting too soon means losing the benefits - and sometimes making things worse. For example, stopping an antidepressant suddenly can trigger withdrawal symptoms that feel like a relapse. Stopping blood pressure meds can spike your risk of stroke. Antibiotics? If you stop early, you could breed resistant bacteria. The goal isn’t to suffer through discomfort. It’s to work with your provider to find a way to stay on track.What to Say Before You Start
Don’t wait until you’re miserable to speak up. When your doctor prescribes a new medication, ask three simple questions:- “What percentage of people experience this side effect?”
- “How long does it usually last?”
- “What can I do to reduce it?”
Track It Like a Pro
Your memory isn’t reliable. You’ll forget when the dizziness hit, how bad it was, or whether it happened after lunch or dinner. That’s why tracking matters. You don’t need a fancy app. A notebook, a notes app on your phone, or even a spreadsheet works. Record:- When - time of day, after which dose
- What - exactly what you felt (e.g., “head pounding,” “stomach cramping”)
- Severity - rate it 1 to 10
- What you did - did you eat? Skip a dose? Drink coffee?
- Impact - did it stop you from working, driving, or sleeping?
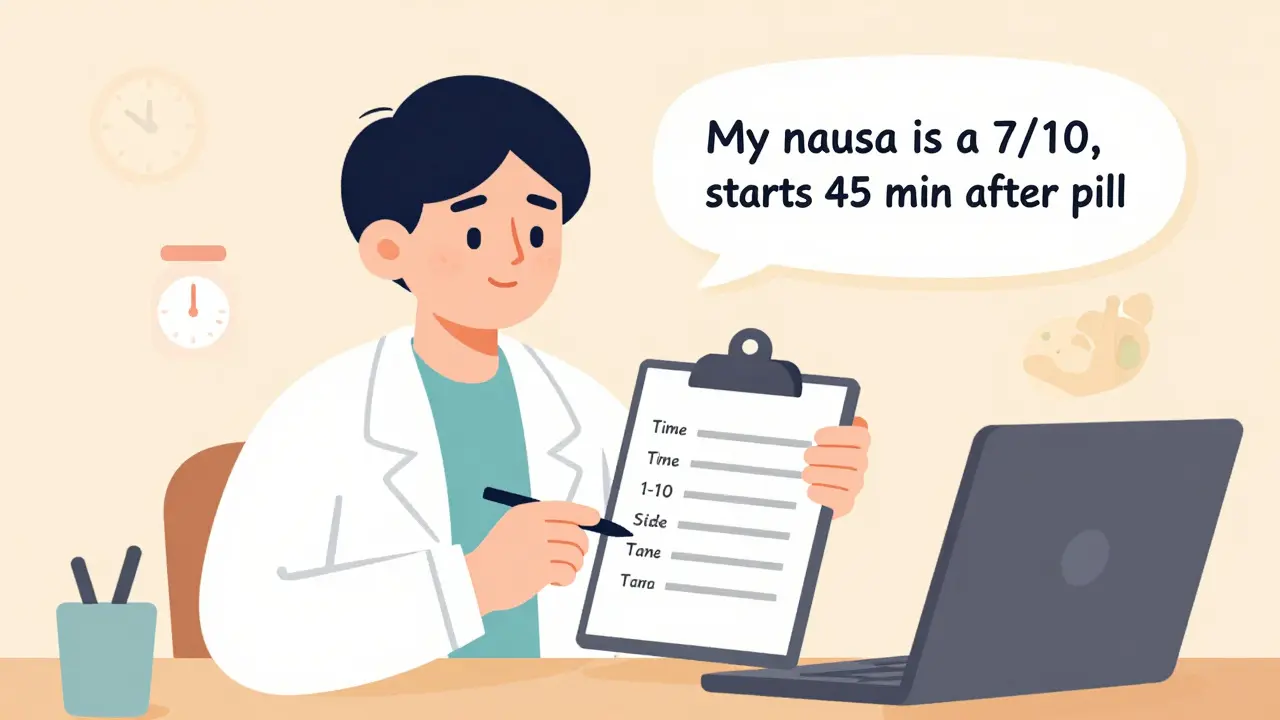
Use the SWIM Framework
When you sit down with your doctor or pharmacist, don’t say, “I feel bad.” Say this:- Severity - “My nausea is a 7/10.”
- When - “It starts 45 minutes after I take the pill.”
- Intensity - “I can’t keep food down. I’ve lost 3 pounds this week.”
- Management - “I’ve tried taking it with toast, but it hasn’t helped. What else can I try?”

Reframe the Side Effect
Here’s something surprising: sometimes, side effects mean the drug is working. A groundbreaking 2021 study published in PMC found that telling patients, “This mild headache or fatigue is a sign the medication is active in your body,” reduced anxiety by 37% and cut discontinuation rates by 29%. That’s not placebo. It’s science. For example, some blood pressure meds cause fatigue because they’re slowing your heart rate - which is the whole point. Antidepressants can cause nausea early on because they’re increasing serotonin - which eventually lifts your mood. It doesn’t mean the drug is failing. It means it’s adjusting. Your provider can help you tell the difference between “normal adjustment” and “dangerous reaction.”Try These Practical Fixes
Before you think about quitting, try these low-risk changes - all of which your provider can approve:- Change the time of day - Take a pill at night instead of morning. Many side effects (like dizziness or fatigue) are less disruptive when you’re asleep.
- Take with food - A small snack can reduce stomach upset. One GoodRx case study showed a patient cut nausea from 6 times a day to 2 after starting to take their med with a banana.
- Split the dose - If you take 20mg once daily, ask if 10mg twice daily is an option. Smaller doses can reduce side effects.
- Add a helper - An anti-nausea pill, a sleep aid, or a stool softener might be all you need. Pharmacists are trained to suggest these.
Know When to Push Back
Not all side effects are manageable. Some are serious. If you experience:- Swelling of the face, lips, or throat
- Severe rash or peeling skin
- Chest pain or irregular heartbeat
- Thoughts of self-harm or suicide
- Jaundice (yellowing of skin or eyes)

What to Bring to Your Appointment
Walk in prepared. Bring:- Your full medication list (including supplements and OTC drugs)
- Your side effect tracker (even if it’s messy)
- Questions written down
- Any pharmacy labels or packaging
It Takes Practice
You won’t get this right on the first try. The NIH found that most people need 2 to 3 conversations before they feel confident talking about side effects. That’s normal. Each time you do it, you get better. You’ll learn what questions to ask. You’ll notice patterns. You’ll realize your provider isn’t dismissing you - they’re trying to help. And with every successful conversation, you’re not just staying on your medication. You’re taking control of your health.What if my side effect is really bad? Should I still keep taking it?
Not all side effects are equal. Mild ones - like dry mouth, mild nausea, or drowsiness - often fade in 1-2 weeks. But if you’re having severe symptoms like chest pain, trouble breathing, swelling, or thoughts of self-harm, stop the medication and contact your provider immediately. For moderate symptoms, don’t quit. Track them, write them down, and bring them to your next appointment. Your provider can adjust your dose, timing, or add a helper medication. Quitting without talking to them risks worse outcomes.
Can I just lower my dose on my own to reduce side effects?
No. Never change your dose without talking to your provider first. Some medications, like blood pressure pills or antidepressants, can cause dangerous withdrawal if stopped or reduced suddenly. Others, like antibiotics, lose effectiveness if not taken as prescribed. Even if you think lowering the dose will help, your provider needs to decide. They might suggest splitting the pill, switching to a different formulation, or adding another drug to offset the side effect. But you don’t get to make that call alone.
Is it true that side effects mean the drug is working?
Sometimes, yes. For example, fatigue from a beta-blocker means your heart rate is slowing - which is the goal. Nausea from an SSRI can mean serotonin levels are rising - which helps depression. This doesn’t mean all side effects are good. But research shows that reframing minor symptoms as signs the drug is active reduces anxiety and helps people stick with treatment. Your provider can help you separate the normal from the dangerous.
I’m embarrassed to talk about side effects. What if my doctor thinks I’m overreacting?
You’re not overreacting. Side effects are real, and they’re one of the top reasons people quit medications. In fact, a Mayo Clinic study found that 61% of people who stopped meds without telling their doctor did so because they thought their provider wouldn’t care. That’s a myth. Most providers want to hear about side effects - it helps them help you. Bring your tracking log. Be specific. Use the SWIM framework. You’re not complaining - you’re problem-solving. And if your provider dismisses you, ask for a referral to a pharmacist or specialist. Medication adherence is their job, too.
Do apps really help with tracking side effects?
Yes. A 2023 JAMA Internal Medicine study found that patients using FDA-authorized medication apps had 18% higher adherence than those who didn’t. Apps like Medisafe, MyTherapy, or even a simple notes app with timestamps help you spot patterns you’d miss otherwise. They also make it easier to show your provider exactly what’s happening. You don’t need a fancy app - just consistent logging. But if you’re already using one, keep going. It’s working.


 Medications
Medications





Jonah Mann
February 7, 2026 AT 13:51Man i just started my new bp med last week and the dizziness is WILD. Thought i was gonna pass out every time i stood up. Almost quit till i read this. Took it at night instead of morning and boom. No more spinning. Like magic. Thanks for the tip.
THANGAVEL PARASAKTHI
February 8, 2026 AT 17:02Really appreciate this. In india, a lot of people just stop meds because they cant afford followups. But the tracking part? Game changer. Even a notebook helps. I showed my aunt her nausea pattern-she took it after dinner, not empty stomach. No more vomiting. Small change, big difference.
Tatiana Barbosa
February 10, 2026 AT 12:57THIS. I was on sertraline for 3 weeks and felt like a zombie. Thought it was broken. Then i tracked: nausea peaked at 90 mins post-pill, fatigue hit at 4pm. I switched to bedtime, added ginger tea, and now i’m sleeping better than ever. Side effects aren’t failures-they’re data points. You’re not broken. Your body’s just adjusting. Keep going.
Ken Cooper
February 11, 2026 AT 09:08Wait-so you’re saying nausea from an SSRI means serotonin’s rising? I thought i was just doomed. My doc never explained that. I’ve been on fluoxetine for 10 days, puked twice, felt like garbage. But now i’m like… maybe it’s working? Like, my brain’s actually rewiring? That’s wild. I’ll keep going. Thanks for reframing it.
Sam Dickison
February 11, 2026 AT 22:43SWIM framework is legit. I used it last month with my pharmacist. Said: severity 8/10, starts 40 min post-dose, intensity = can’t eat, management = tried with food, no help. She switched me from once-daily to split dose. No more stomach cramps. Also, she gave me a free anti-nausea sample. Pharmacist > doctor sometimes. Just saying.
John McDonald
February 12, 2026 AT 01:21My wife quit her diabetes med because of dry mouth. Thought it was ‘just annoying.’ Lost 12 lbs in 3 weeks. Ended up in the ER. We didn’t know dry mouth could mean dehydration + high glucose. Now she tracks everything. Uses a notes app. Takes it with meals. No more crashes. You’re not overreacting. You’re surviving.
Joshua Smith
February 12, 2026 AT 06:16One thing i didn’t see mentioned: what if you’re on 3+ meds? Tracking gets messy. I tried a spreadsheet, but it was overwhelming. Ended up using color-coded stickers on my pillbox. Red = dizziness, blue = nausea, green = fine. Showed it to my doc. She spotted a pattern with my statin and antihistamine. Changed timing. Done. Simple. No app needed.
Jessica Klaar
February 13, 2026 AT 23:41I’m a nurse and i’ve seen this a hundred times. People think their provider will judge them. But honestly? We want to hear it. The more detail, the better. One patient brought me a hand-drawn chart with times, meals, and even weather. I cried. Not because it was perfect-because it was honest. You’re not a burden. You’re a partner.
glenn mendoza
February 14, 2026 AT 04:41It is imperative that individuals recognize the physiological significance of adverse reactions in the context of pharmacological intervention. The cessation of therapeutic regimens without professional consultation constitutes a significant risk to homeostatic equilibrium. Empirical evidence supports the assertion that structured communication with healthcare providers enhances therapeutic adherence and mitigates iatrogenic complications. Therefore, a systematic approach to symptom reporting is not merely advisable-it is clinically essential.
John Watts
February 14, 2026 AT 17:24Bro i just started metformin. Thought i was dying. Diarrhea every 2 hours. Almost quit. Then i read this. Took it with dinner. Added a probiotic. Now it’s just a little tummy rumble. I’m alive. I’m stable. I’m not quitting. This article saved me. Thank you.
Randy Harkins
February 15, 2026 AT 19:52Love this 💯 I’ve been on lithium for 3 years. The hand tremors? Annoying. But now i know they mean it’s working. I track ‘em. I show my psych. She adjusts my dose. I’m stable. No hospital stays. No quitting. Just science + patience. You got this 🙌
Chima Ifeanyi
February 17, 2026 AT 17:15Interesting how this assumes everyone has access to a doctor, a pharmacy, a phone, or even a notebook. In real life, 60% of people don’t. You’re preaching to the privileged. My cousin took her antihypertensive and got dizzy. She didn’t have a car. Couldn’t afford the followup. She stopped. Died last year. This isn’t empowerment. It’s a luxury.
Angie Datuin
February 18, 2026 AT 11:52I used to think side effects meant the drug wasn’t right for me. Now i know they’re just the body saying ‘hold on, we’re adjusting.’ I track everything. Even the weird dreams. My doc laughs at my notes. But she changes things. I’m healthier than i’ve been in years. Just… keep going.
Camille Hall
February 19, 2026 AT 08:15Just one sentence: Don’t quit. Talk. Track. Adjust. You’re not weak for feeling side effects-you’re strong for staying.