Statin Myopathy Risk Calculator
This tool assesses your risk of developing statin-induced muscle pain and weakness based on key factors discussed in the article. Understanding your personal risk can help you make informed decisions with your doctor about statin therapy.
For millions of people, statins are a lifeline. They lower cholesterol, prevent heart attacks, and save lives. But for a significant number of users, that lifeline comes with a heavy cost: muscle pain, weakness, and fatigue. This isn’t just a minor inconvenience. It’s a real, measurable condition called statin-induced myopathy, and it’s more common than most doctors admit.
If you’ve started a statin and suddenly feel like your legs are made of lead, or you can’t climb stairs without stopping, you’re not imagining it. You’re not weak. You’re not lazy. Your muscles are reacting to a biochemical shift triggered by the drug itself. And understanding how this happens is the first step to fixing it.
How Statins Actually Damage Muscle Tissue
Statins work by blocking HMG-CoA reductase, an enzyme in the liver that makes cholesterol. But they don’t just stop there. They also block the production of other vital molecules - ones your muscles need to function properly. This is where the trouble starts.
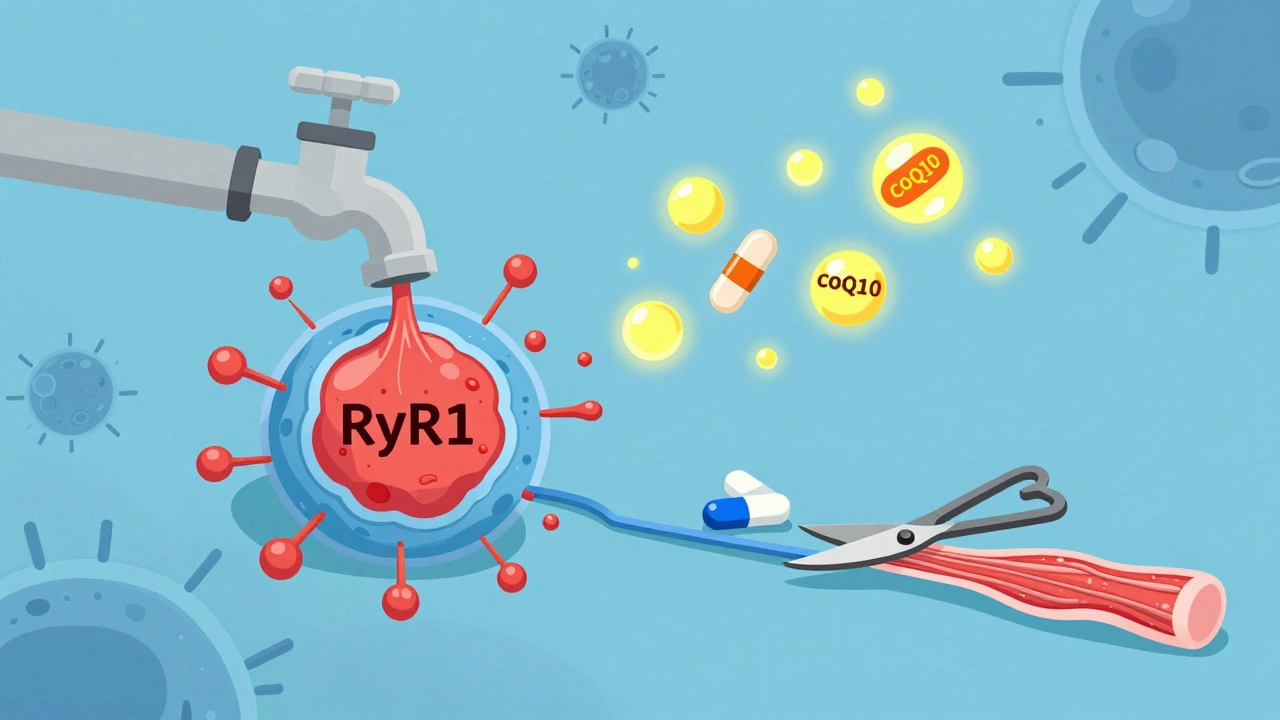
One of the most damaging effects is what happens to calcium inside muscle cells. Every muscle contraction relies on precise calcium signals. In healthy muscle, calcium is tightly controlled. But statins cause a protein called FKBP12 to detach from the ryanodine receptor (RyR1), a calcium channel in muscle cells. Without FKBP12 holding it steady, the channel leaks calcium like a broken faucet. Studies show this leak increases by 2.3 times in people taking statins. That constant calcium flood triggers a chain reaction: enzymes called calpains and caspase-3 get activated, which start breaking down muscle fibers. It’s like your body is slowly digesting its own muscle tissue.
Then there’s CoQ10. This molecule is essential for energy production in mitochondria - the power plants of your cells. Statins reduce CoQ10 levels in muscle tissue by about 40% within just four weeks. Without enough CoQ10, your muscles can’t make energy efficiently. They fatigue faster, recover slower, and produce more damaging free radicals. That’s why many people feel exhausted, even if they’re not doing anything unusual.
And here’s something most people don’t know: about 5-10% of persistent cases aren’t just chemical side effects. They’re autoimmune. The body starts making antibodies against its own HMG-CoA reductase enzyme - the very target of the statin. This form, called anti-HMGCR myositis, is rare but severe. It doesn’t go away when you stop the statin. It needs immunosuppressants like prednisone and methotrexate to calm down.
Who’s Most at Risk?
Not everyone on statins gets muscle problems. But some groups are far more vulnerable.
Older adults - especially women over 65 - are at higher risk. So are people with smaller body frames, kidney or liver disease, or those taking multiple medications. Certain statins are worse than others. Simvastatin and lovastatin carry the highest risk. Atorvastatin and rosuvastatin are a bit safer, but still cause issues in many people.
Genetics also play a role. People with a specific variant of the SLCO1B1 gene have trouble clearing statins from their blood, leading to higher concentrations and more muscle exposure. A simple genetic test can reveal this risk before you even start the drug.
And then there’s exercise - or the lack of it. Sedentary people are more likely to develop symptoms. But here’s the twist: moderate exercise doesn’t make it worse. It helps.
The Exercise Myth - Why Moving More Can Save Your Muscles
For years, doctors told people with statin muscle pain to rest. That advice is wrong.
A 2021 Mayo Clinic study found that patients who walked 30 minutes a day, five days a week, reported 41% fewer muscle symptoms than those who stayed inactive. Why? Because movement helps restore FKBP12 binding to the RyR1 channel. In animal studies, rats that ran on wheels showed normal calcium control even while on statins. Human trials confirmed it: after eight weeks of consistent, moderate exercise, 72% of participants had their calcium leaks reduced to normal levels.
You don’t need to run marathons. Just keep moving. Walk. Swim. Ride a bike. Gardening counts. The goal isn’t intensity - it’s consistency. Movement keeps the calcium channels stable and improves mitochondrial function, helping your muscles cope with the statin’s effects.

What to Do When Muscle Pain Hits
If you start feeling muscle pain, weakness, or cramps within the first six months of starting a statin, don’t ignore it. Don’t just push through. Don’t assume it’s aging.
First, get a blood test for creatine kinase (CK). Levels above 10 times the upper limit of normal confirm true myopathy. Even if CK is normal, persistent symptoms still matter. Many people have symptoms without elevated CK - that’s called statin-associated muscle symptoms (SAMS), and it’s still real.
Next, try a statin washout. Stop the drug for 4 weeks. If your symptoms improve, it’s likely the statin. About 80% of people see improvement within that time.
Now comes the hard part: deciding what to do next.
Alternatives That Work Without Destroying Muscle
You don’t have to give up on lowering your cholesterol just because statins hurt your muscles.
CoQ10 supplementation is the most studied option. A 2022 European study showed 200 mg per day reduced muscle pain in 35% of patients. Some report feeling better in as little as two weeks. It’s not a cure, but it’s a powerful tool.
Ezetimibe lowers LDL cholesterol by about 30% by blocking cholesterol absorption in the gut. It doesn’t affect muscle cells. In trials, muscle side effects were nearly identical to placebo.
PCSK9 inhibitors like evolocumab are injectable drugs that slash LDL by 60% or more. In the FOURIER trial, only 3.7% of users reported muscle issues - lower than the placebo group. The catch? They cost about $5,850 a year. But for people with severe statin intolerance and high heart risk, they’re often worth it.
And if you have anti-HMGCR antibodies? That’s a different ballgame. You’ll need immunosuppressive therapy. Methotrexate and prednisone can bring remission in 68% of cases within six months. But you must get tested for these antibodies if symptoms persist after stopping statins.
What Doesn’t Work
Don’t waste time on unproven fixes. Magnesium? Vitamin D? Turmeric? They might help general inflammation, but they don’t fix the core problem - calcium leaks, CoQ10 depletion, or autoimmunity.
Also, don’t switch to a different statin hoping it’ll be better. Only about 40% of people tolerate a switch. Reducing the dose helps 65% of the time, but you may not get enough cholesterol control.
And avoid the myth that “all statins are the same.” They’re not. Simvastatin is the worst offender. Pravastatin and fluvastatin are gentler on muscles. But even the safest ones can cause problems in susceptible people.
The Bigger Picture
Statins are prescribed to 39 million Americans. About 6 million of them experience muscle symptoms each year. That’s a lot of people feeling sidelined by a drug meant to save them.
The medical community is waking up. The American College of Cardiology now recommends discussing muscle risks before prescribing. Doctors are more likely to test for genetic risk factors and offer alternatives upfront.
New drugs are coming. Two experimental statins - STT-101 and STT-202 - are designed to target the liver while avoiding muscle tissue. Early results show 70% less muscle exposure. If they work in humans, they could change everything.
But until then, the best tools we have are simple: test your CK, try CoQ10, move your body, and know your options. You don’t have to choose between heart health and muscle function. There’s a middle path - if you know where to look.
Can statin muscle pain go away on its own?
Yes, in most cases. If you stop taking the statin, symptoms usually improve within 1 to 4 weeks. About 80% of people see noticeable relief after a 4-week washout period. But if symptoms persist beyond that, it could be a sign of a more serious issue, like autoimmune myositis, which requires medical treatment.
Is CoQ10 really effective for statin muscle pain?
Yes, for many people. Clinical trials show that taking 200 mg of CoQ10 daily reduces muscle pain and weakness in about 35% of statin users. It works by restoring mitochondrial energy production and reducing oxidative stress in muscle cells. While it won’t fix everything, especially in autoimmune cases, it’s one of the safest and most evidence-backed options available.
Should I stop my statin if I have muscle pain?
Don’t stop on your own. Talk to your doctor first. Stopping statins without a plan can raise your risk of heart attack or stroke, especially if you’ve had one before. Your doctor can help you test for statin-related causes, try a washout, and explore safer alternatives. The goal is to protect your heart without damaging your muscles.
Can exercise make statin muscle pain worse?
No - it usually helps. Studies show that moderate exercise like brisk walking 150 minutes per week reduces muscle symptoms by up to 41%. It helps stabilize calcium channels in muscle cells and improves energy production. Avoid intense weightlifting or sudden high-intensity workouts if you’re in pain, but don’t stop moving. Movement is part of the treatment.
Are there statins that are easier on muscles?
Yes. Pravastatin and fluvastatin are generally better tolerated than simvastatin or lovastatin. Atorvastatin and rosuvastatin fall in the middle. But even the gentler ones can cause problems in people with genetic risk factors or other health conditions. The key isn’t just which statin - it’s whether your body can handle it at all. Testing for SLCO1B1 gene variants can help predict this.
What is anti-HMGCR myositis?
It’s a rare autoimmune condition triggered by statins in about 0.02% of users. The body produces antibodies against its own HMG-CoA reductase enzyme, leading to severe, persistent muscle inflammation that doesn’t improve after stopping the drug. Symptoms include progressive weakness, especially in hips and shoulders. Diagnosis requires a blood test for anti-HMGCR antibodies. Treatment involves immunosuppressants like prednisone and methotrexate, and recovery can take months.
Can I ever go back on statins after muscle pain?
Maybe - but not always. About 40% of people can tolerate a different statin at a lower dose after a washout. Some can return to statins if they take CoQ10 and exercise regularly. But if you had autoimmune myositis or severe symptoms with elevated CK, returning to statins is usually not recommended. Alternatives like ezetimibe or PCSK9 inhibitors are safer long-term options.


 Medications
Medications




Webster Bull
December 14, 2025 AT 10:47Statins wreck muscles? No shit. I took simvastatin for 3 months and couldnt lift my damn grocery bags. Walked 20 mins a day, popped 200mg CoQ10, and boom - legs came back. Doctors need to stop acting like its all in our heads.
kevin moranga
December 15, 2025 AT 06:31Man, this post hit home. I was on atorvastatin for 5 years - started with mild cramps, then my quads felt like wet cardboard. I thought I was just getting old. Turns out, my CK was 800. Doctor said 'just push through.' Push through what? My dignity? I stopped, did the 4-week washout, started walking daily, and took CoQ10. Within 6 weeks, I was hiking again. Not saying statins are evil - but they're not harmless either. Your muscles aren't just 'weak' - they're under biochemical siege. And movement? It's not a suggestion. It's medicine. I wish I'd known this sooner. If you're reading this and feeling like your body's betraying you - you're not crazy. You're just getting the side effects no one talks about. And yes, it can get better. It did for me.
Emma Sbarge
December 16, 2025 AT 12:18So let me get this straight - we're telling people to take a drug that sabotages their muscle cells, then telling them to walk it off? And the solution is to spend $6k/year on injections? This isn't healthcare. This is a corporate circus. I'm not anti-medication. I'm pro-common-sense. If a drug makes you feel like you're turning to jelly, maybe it's not the right drug for you. Period.
Donna Hammond
December 17, 2025 AT 05:38Thank you for writing this with such clarity. I'm a physical therapist and see this every week - patients who’ve been told their muscle pain is 'just aging' or 'lack of fitness.' The science here is solid: calcium leakage, CoQ10 depletion, and autoimmune triggers are real mechanisms, not anecdotes. I recommend CoQ10 200mg daily to all statin users, and I emphasize movement - not as punishment, but as protection. The Mayo Clinic study is gold. Also, genetic testing for SLCO1B1 is underused. If your doctor won’t order it, ask for it. Your muscles will thank you.
Lauren Scrima
December 18, 2025 AT 13:53Oh wow. So instead of just popping a pill like a good little American, we’re supposed to… walk? Take a supplement? Maybe not die on the hill of 'statins are the only option'? I’m shocked. Shocked, I tell you.
Harriet Wollaston
December 20, 2025 AT 06:47This is the kind of post that makes me feel less alone. My mom had statin myopathy - she couldn’t get out of her chair without help. We tried everything. CoQ10 helped a little. But the real turning point? Swimming. Just 20 minutes, 3x a week. She said it felt like her muscles remembered how to work. I’m so glad someone’s finally talking about the real solutions - not just the pharmaceutical ones.
Richard Ayres
December 20, 2025 AT 20:01The complexity of this issue deserves more attention. Statins are a double-edged sword: life-saving for some, debilitating for others. The fact that we now understand the biochemical pathways - calcium dysregulation, mitochondrial dysfunction, and autoimmune cross-reactivity - shows how far pharmacology has come. Yet, our clinical practices lag behind. We need more routine screening, personalized dosing, and non-statin alternatives as first-line options for high-risk populations. This isn't about fear-mongering; it's about precision medicine. We owe our patients better than a one-size-fits-all approach.
Scott Butler
December 22, 2025 AT 05:51So now we're blaming Big Pharma for people being lazy? I've seen guys on statins who can't climb stairs - but they sit on their couch watching ESPN all day. Move? Yeah, right. Get off your butt and do something. No drug is perfect, but you want to live past 60? Take the pill. And stop whining.
sharon soila
December 23, 2025 AT 07:25Let me say this with love and care: your body is a temple. Statins are not the answer for everyone. Walking every day is not a chore - it is a gift. CoQ10 is not a supplement - it is a restoration. You are not broken. You are not failing. You are simply being asked to listen - and to move - in a way that honors your biology. There is peace in this path. There is strength. And there is hope.
Bruno Janssen
December 23, 2025 AT 16:03I took rosuvastatin. My legs turned to jelly. I stopped. I felt better. But now I'm terrified I'm gonna have a heart attack. What if I die because I listened to this post? What if I'm just weak? Why does everything have to be so complicated?