Peripartum cardiomyopathy (PPCM) is a rare but serious heart condition that strikes women in the last month of pregnancy or up to five months after giving birth. The heart weakens, pumps less blood, and fluid can build up in the lungs and legs. It’s not common - about 1 in 1,000 to 4,000 deliveries - but when it happens, it’s life-threatening. Treatment focuses on easing symptoms, improving heart function, and preventing complications. Among the drugs used, digoxin plays a specific, though limited, role.
What Is Digoxin and How Does It Work?
Digoxin is a cardiac glycoside derived from the foxglove plant. It’s been used for over 200 years to treat heart failure and certain irregular heart rhythms. It works in two main ways: it slows down the heart rate by affecting the AV node, and it makes the heart muscle contract more forcefully. This helps the heart pump more efficiently, even when it’s weakened.
In modern cardiology, digoxin isn’t a first-line drug for heart failure anymore. Guidelines from the American Heart Association and European Society of Cardiology now favor ACE inhibitors, beta-blockers, and SGLT2 inhibitors as primary treatments. But digoxin still has a place - especially when those drugs aren’t enough to control symptoms or heart rate.
Why Digoxin Is Considered in Peripartum Cardiomyopathy
PPCM patients often have both reduced pumping ability and fast heart rates. Some develop atrial fibrillation, a dangerous irregular rhythm that worsens heart failure. In these cases, digoxin helps by slowing the heart rate without depressing heart function too much - something some other rate-control drugs can do.
Unlike beta-blockers, which may cross the placenta and affect the fetus in late pregnancy, digoxin has a long safety record in pregnancy. Studies show it doesn’t increase birth defects or miscarriage risk when used at therapeutic doses. That makes it one of the few heart failure drugs that can be safely continued during pregnancy and after delivery.
Also, digoxin doesn’t cause low blood pressure or fatigue as often as other medications. For new mothers who need to care for a newborn, maintaining energy levels matters. Digoxin’s mild effect on blood pressure can be an advantage in this group.
When Digoxin Is Actually Used - Not Just Prescribed
Digoxin isn’t given to every PPCM patient. It’s reserved for those who:
- Still have symptoms like shortness of breath or swelling despite being on standard therapy (diuretics, beta-blockers, ACE inhibitors)
- Have persistent atrial fibrillation with a fast ventricular rate
- Can’t tolerate beta-blockers due to low blood pressure or asthma
Research from the University of Pennsylvania’s PPCM registry (2023) tracked 187 women with confirmed PPCM. Of those, only 28% received digoxin. Among them, 62% showed improvement in ejection fraction over six months - similar to those not on digoxin. But the digoxin group had better control of heart rate and fewer hospital readmissions for heart failure flare-ups.
This suggests digoxin doesn’t fix the underlying heart damage - but it helps manage symptoms and keeps things stable while the heart recovers.
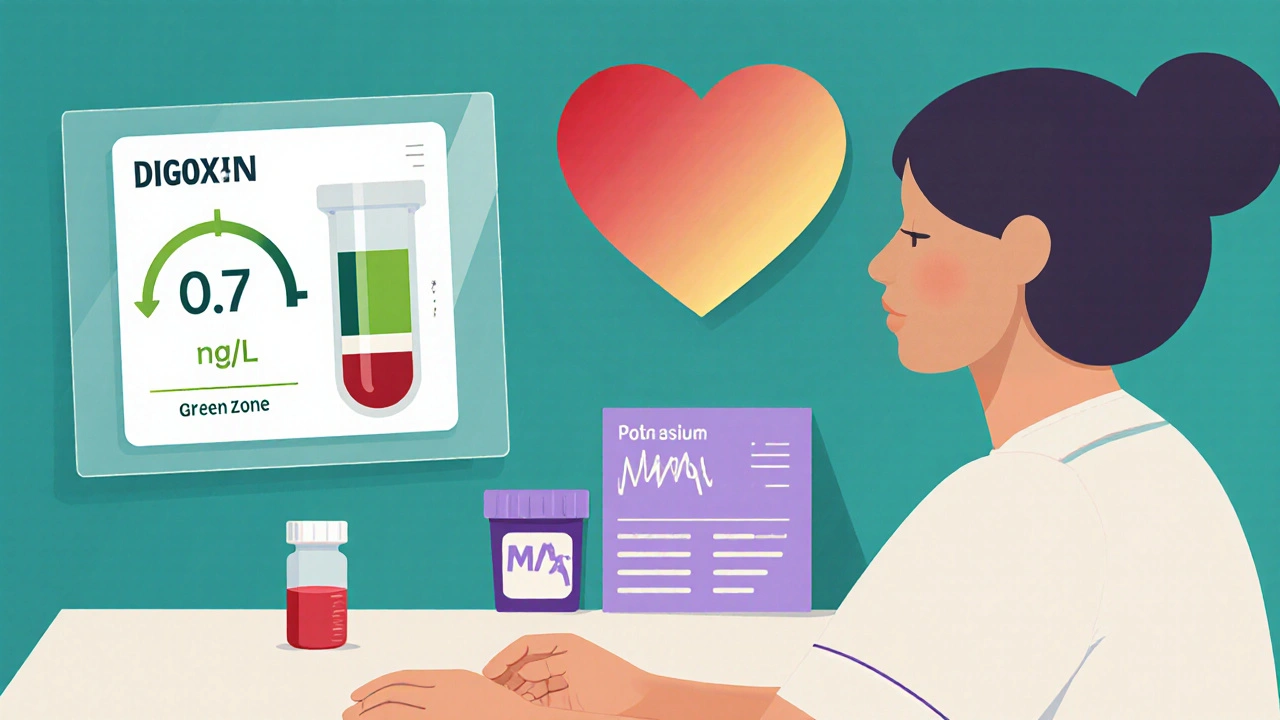
Dosing and Monitoring: The Critical Details
Digoxin is not a drug you can guess with. The difference between a helpful dose and a toxic one is tiny. In PPCM, doctors usually start with 0.125 mg once daily. For women with kidney problems - common after pregnancy - the dose may be cut to 0.0625 mg.
Why? Because digoxin is cleared by the kidneys. After delivery, kidney function can still be impaired, especially if the mother had preeclampsia. A standard adult dose could build up and cause poisoning.
Signs of digoxin toxicity include nausea, vomiting, blurry yellow-green vision, confusion, and irregular heartbeat. If any of these show up, the drug is stopped immediately. Blood tests for digoxin levels are done routinely - target range is 0.5 to 0.9 ng/mL. Levels above 1.2 ng/mL are dangerous.
Other medications can interfere. Diuretics like furosemide can lower potassium, which makes digoxin more toxic. Magnesium and potassium supplements are often given alongside digoxin in PPCM patients to prevent this.
Digoxin vs. Other Heart Failure Drugs in PPCM
Here’s how digoxin compares with other common treatments:
| Medication | Use in Pregnancy | Effect on Ejection Fraction | Heart Rate Control | Risk of Toxicity |
|---|---|---|---|---|
| Digoxin | Safe | Mild improvement | Good | High (narrow window) |
| Beta-blockers (e.g., metoprolol) | Generally safe | Significant improvement | Excellent | Low |
| ACE inhibitors (e.g., lisinopril) | Not safe in pregnancy | Significant improvement | Minimal | Low |
| SGLT2 inhibitors (e.g., dapagliflozin) | Not studied in pregnancy | Strong improvement | Minimal | Low |
| Diuretics (e.g., furosemide) | Safe | No direct effect | No | Low (electrolyte imbalance) |
As the table shows, digoxin doesn’t improve heart function as much as beta-blockers or SGLT2 inhibitors. But it’s one of the few options that can be used safely throughout pregnancy and postpartum while also controlling heart rate. That’s why it’s still in the toolkit.
Real-World Use: What Doctors Actually Do
In clinical practice, most PPCM patients get beta-blockers and diuretics first. If they’re still symptomatic after 2-4 weeks, doctors may add digoxin - especially if the heart rate is above 90 beats per minute at rest.
One case from a Bristol maternity unit in 2024 involved a 32-year-old woman who developed PPCM two weeks after a C-section. Her ejection fraction was 28%. She was on metoprolol and furosemide but still had palpitations and fatigue. Her heart rate stayed at 110 bpm. Digoxin was started at 0.0625 mg daily. Within three weeks, her heart rate dropped to 78 bpm, and she could walk up one flight of stairs without gasping. Her ejection fraction improved to 38% by six months.
She didn’t need an implantable defibrillator or advanced therapies. Digoxin helped bridge her to recovery.
When Digoxin Should Be Avoided
Digoxin isn’t for everyone. It’s not recommended if:
- The patient has ventricular tachycardia (not atrial fibrillation)
- Kidney function is severely impaired (eGFR below 30 mL/min)
- There’s a history of digoxin toxicity
- The patient is taking drugs like clarithromycin or verapamil, which raise digoxin levels
Also, if the heart function recovers quickly - which happens in about 50% of PPCM cases within six months - digoxin is usually stopped. There’s no need to keep taking it long-term if the heart heals.
Long-Term Outlook and Recovery
Many women with PPCM recover fully. About half regain normal heart function within six months. For those who don’t, digoxin may be needed longer - sometimes permanently. But it’s rarely the only drug used in chronic cases. Newer medications like SGLT2 inhibitors are now being studied in post-PPCM patients, and early results look promising.
Digoxin’s role is not to cure PPCM. It’s to help women survive the acute phase, feel better while their heart heals, and avoid dangerous rhythms. It’s a bridge, not a destination.
Is digoxin safe to take while breastfeeding?
Yes, digoxin is considered safe during breastfeeding. Less than 1% of the maternal dose passes into breast milk, and it’s poorly absorbed by the baby’s gut. No adverse effects have been reported in nursing infants. Still, babies should be monitored for signs of toxicity like poor feeding or unusual tiredness - though this is extremely rare.
Can digoxin cause miscarriage or birth defects?
No large studies have linked digoxin to miscarriage or birth defects. It’s classified as Pregnancy Category C, meaning animal studies showed some risk, but human data are reassuring. Over 1,000 pregnancies exposed to digoxin show no increase in congenital anomalies. It’s one of the safest heart drugs to use during pregnancy when needed.
Why not use a different drug instead of digoxin?
Other drugs like beta-blockers do a better job at improving heart function and are preferred first-line. But they don’t always control heart rate well enough, especially in atrial fibrillation. Digoxin fills that gap. It’s also one of the few options that can be used safely during pregnancy - unlike ACE inhibitors or SGLT2 inhibitors, which are avoided entirely.
How long do women typically take digoxin for PPCM?
Most women take digoxin for 3 to 6 months. If heart function improves - measured by echocardiogram - the drug is gradually tapered and stopped. If the heart doesn’t recover, digoxin may be continued long-term, often alongside newer medications like SGLT2 inhibitors. It’s not a lifelong drug for most, but it’s critical during the recovery window.
Can digoxin be used with other heart failure drugs?
Yes, it’s often used with beta-blockers, diuretics, and sometimes spironolactone. But it’s not combined with drugs that raise its blood level, like amiodarone or verapamil. Always check for interactions. Blood tests for potassium, magnesium, and digoxin levels are essential when using it with other heart meds.



 Medications
Medications




Hope NewYork
November 2, 2025 AT 01:16Bonnie Sanders Bartlett
November 3, 2025 AT 21:03Melissa Delong
November 5, 2025 AT 03:49Marshall Washick
November 7, 2025 AT 02:11Abha Nakra
November 8, 2025 AT 21:19Neal Burton
November 10, 2025 AT 02:04Tamara Kayali Browne
November 10, 2025 AT 19:33Lori Johnson
November 12, 2025 AT 08:02Tatiana Mathis
November 14, 2025 AT 05:27Michelle Lyons
November 15, 2025 AT 11:39Cornelle Camberos
November 16, 2025 AT 14:16joe balak
November 17, 2025 AT 21:22