TZD Fluid Retention Calculator
Estimate how much of your weight gain is likely fluid retention and assess your risk level
Fluid Retention Estimate
Based on your input:
- Estimated fluid gain: lbs
- Estimated fat gain: lbs
- Fluid retention percentage: %
Your next steps:
Warning: This level of fluid gain is significant. Consult your doctor immediately.
When you're taking a diabetes medication like pioglitazone or rosiglitazone, the goal is simple: better blood sugar control. But for many people, the trade-off isn't worth it. TZD weight gain and swelling in the ankles and feet are common-and sometimes severe-side effects that lead people to stop taking these drugs altogether. You're not alone if you've seen the scale climb by 5 or 6 pounds in a few weeks, or if your shoes feel tighter than they used to. These aren't just annoyances. They're signs of fluid retention that can put real strain on your heart.
Why TZDs Cause Weight Gain and Swelling
TZDs work by making your body more sensitive to insulin. That’s great for lowering blood sugar, especially if you have deep insulin resistance. But here’s the catch: the same mechanism that helps your muscles use glucose better also tells your kidneys to hold onto sodium and water. That’s where the weight comes from-not fat, mostly. Studies show that 65% to 70% of the weight gain from TZDs is actually fluid, not fat. The rest comes from increased fat storage under the skin, especially in the hips and thighs.
This isn’t just a minor side effect. In clinical trials, about 5% of people on TZDs alone developed noticeable swelling. When combined with insulin, that number jumps to over 15%. For someone already managing heart risks or kidney issues, that extra fluid can be dangerous. The FDA added a black box warning in 2007: don’t use TZDs if you have moderate to severe heart failure (NYHA Class III or IV). That’s because extra fluid increases pressure on the heart, making it work harder.
Who’s Most at Risk?
Not everyone on TZDs gets swollen ankles. But some people are far more likely to. If you’re older, have kidney problems, or already have heart disease, your body is less able to handle the extra fluid. Women tend to see more swelling than men, possibly due to hormonal differences in how sodium is processed. People taking higher doses-like 45 mg of pioglitazone-are at much greater risk than those on 15 mg. In one study, edema dropped from 4.8% at 15 mg to 10.2% at 45 mg.
Also, if you’re on insulin at the same time, your risk doubles. Insulin itself causes fluid retention. When you add TZDs on top, the effect isn’t just added-it’s multiplied. That’s why doctors now avoid combining them unless absolutely necessary.
What You Can Do: Practical Strategies
Stopping your medication isn’t always the answer. If TZDs are helping your blood sugar stay steady and other drugs aren’t working, there are ways to reduce the side effects without giving up the benefits.
1. Start Low, Go Slow
Don’t begin with the highest dose. Start with pioglitazone 15 mg once a day. Many people find this enough to control blood sugar without major swelling. If your doctor wants to increase it, wait at least 4-6 weeks before doing so. This gives your body time to adjust. Most side effects show up in the first 4-8 weeks. If you haven’t gained weight or swollen by then, you’re likely in the clear.
2. Monitor Your Weight Daily
Keep a small scale by your bed. Weigh yourself every morning, right after using the bathroom and before eating or drinking. Write it down. If you gain more than 2-3 pounds in a week, that’s a red flag. It’s not normal weight gain-it’s fluid. Call your doctor. Early action can prevent hospitalization. One study showed that people who tracked their weight daily had 34% fewer heart failure hospitalizations.
3. Watch Your Salt Intake
Sodium is the enemy here. Aim for less than 2,000 mg per day. That means no processed foods, no canned soups, no fast food, and no adding extra salt to meals. Read labels. Even bread and cheese can be loaded with sodium. Try herbs, lemon juice, or vinegar for flavor instead. A simple switch like this can reduce swelling by nearly 30%, according to research in the Journal of Diabetes and Its Complications.
4. Elevate Your Legs and Move
When you sit or lie down, prop your feet up. Even 15-20 minutes a few times a day helps fluid drain from your legs. Don’t sit with your legs crossed-it traps fluid. Gentle movement like walking or stretching also helps your circulation. You don’t need to run a marathon. Just avoid being still for long periods.
5. Consider SGLT2 Inhibitors Together
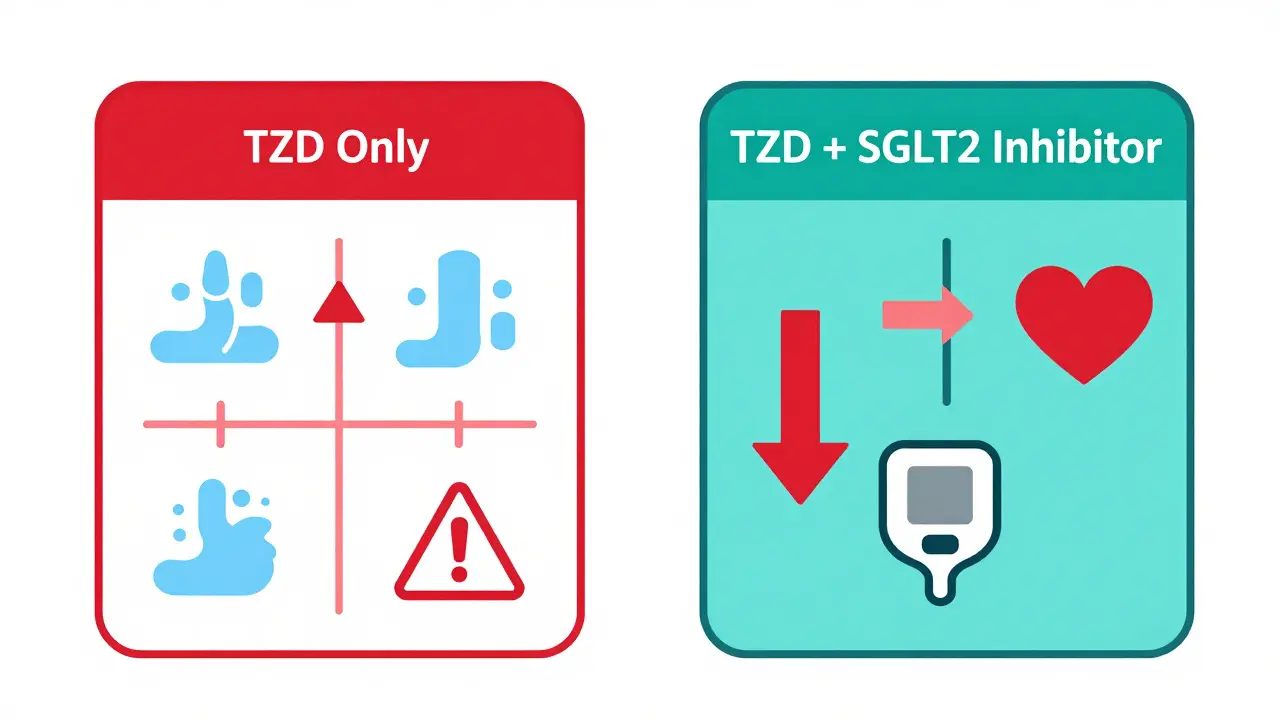
This might sound surprising, but adding an SGLT2 inhibitor like empagliflozin or dapagliflozin can actually reduce TZD-related swelling. These drugs make your kidneys flush out sugar-and sodium-through urine. In clinical trials, combining them with TZDs cut edema risk by 45%. That’s a huge win. Plus, SGLT2 inhibitors help with weight loss and protect your heart. Many doctors now use this combo intentionally, even though it’s not the first choice for everyone.
6. Talk About Diuretics
If you’re still swelling despite lifestyle changes, your doctor might suggest a low-dose diuretic. Thiazides like hydrochlorothiazide are preferred over loop diuretics like furosemide because they’re gentler and less likely to cause electrolyte imbalances. But diuretics aren’t a cure-all. They can make you dehydrated or dizzy. Use them only under close supervision.

What About Other Diabetes Medications?
If side effects are too much, it’s worth asking whether you can switch. Metformin is still the first-line drug for a reason-it doesn’t cause weight gain. In fact, many people lose a few pounds on it. GLP-1 agonists like semaglutide or liraglutide help you lose weight and protect your heart. SGLT2 inhibitors do the same. These newer drugs have replaced TZDs for most people.
TZDs are now considered third-line therapy. That means they’re only used if metformin and one of the newer drugs haven’t worked well enough-and you have severe insulin resistance. If you’re not in that group, there are safer, more effective options.
When to Stop
There are clear signs you should stop TZDs immediately:
- Weight gain over 5 pounds in one week
- Swelling in your legs, feet, or abdomen that doesn’t go down
- Shortness of breath when lying flat or walking short distances
- Feeling unusually tired or dizzy
These aren’t just side effects-they’re warning signs of heart failure. Don’t wait. Call your doctor or go to urgent care. Even if you feel fine, unexplained swelling needs evaluation.
The Bigger Picture
TZDs aren’t gone from medicine-they’re just used much less often. In 2006, they made up nearly 18% of type 2 diabetes prescriptions in the U.S. By 2022, that number dropped to under 5%. Why? Because we now have better tools. Newer drugs don’t just control blood sugar-they protect your heart, kidneys, and weight.
Still, for a small group of people-those with severe insulin resistance who haven’t responded to anything else-TZDs can be a lifeline. The key is using them smartly: low dose, close monitoring, and combining them with other drugs that counteract their downsides.
If you’re on a TZD and you’re worried about swelling or weight gain, talk to your doctor. Don’t assume it’s just "normal." There are real ways to manage it. And if you’re not getting the results you want, ask about alternatives. You deserve a treatment plan that works for your body-not one that just lowers your A1C at the cost of your comfort-or your health.
Is weight gain from TZDs just fat, or is it fluid?
Most of the weight gain from TZDs-about 65% to 70%-is fluid retention, not fat. The rest comes from increased fat storage under the skin. This is why sudden weight gain (over 2-3 pounds a week) is a red flag, even if you haven’t changed your diet.
Can I still take TZDs if I have high blood pressure?
High blood pressure alone doesn’t rule out TZDs, but it does raise your risk of fluid overload. Your doctor will need to monitor you closely. If your blood pressure is hard to control or you have signs of heart strain, TZDs may not be safe. Always check your heart function before starting.
Do all TZDs cause the same side effects?
Rosiglitazone and pioglitazone cause similar levels of weight gain and swelling. But pioglitazone has a better safety record for the heart. Rosiglitazone was restricted in the past due to heart attack concerns, though later studies were less clear. Most doctors now choose pioglitazone if they must use a TZD.
How long does it take for swelling to go away after stopping TZDs?
Most people notice improvement within a few days of stopping TZDs. Swelling usually resolves completely in 1-3 weeks as the body flushes out the extra fluid. If swelling persists beyond a month, you should be checked for other causes like heart or kidney problems.
Are there any new drugs that replace TZDs without the side effects?
Yes. SGLT2 inhibitors (like empagliflozin) and GLP-1 receptor agonists (like semaglutide) now lead the way. They lower blood sugar, help you lose weight, and protect your heart and kidneys. Newer PPAR modulators, like saroglitazar, are being studied and show promise with much less fluid retention, but they’re not yet approved in the U.S. or U.K.
Can lifestyle changes alone fix TZD-related swelling?
Lifestyle changes-like reducing salt, elevating your legs, and daily weight checks-can significantly reduce swelling. In studies, they lowered edema severity by nearly 30%. But they won’t eliminate it completely if you’re still taking the drug. They work best as part of a broader strategy, including dose reduction or adding SGLT2 inhibitors.
What’s Next?
If you’re on a TZD and dealing with swelling or weight gain, your next step is simple: talk to your doctor. Bring your weight logs. Mention any swelling you’ve noticed. Ask if switching to an SGLT2 inhibitor or GLP-1 agonist is an option. You don’t have to accept side effects as part of the deal. Better tools exist. You just need to ask for them.



 Medications
Medications





Mussin Machhour
December 25, 2025 AT 08:56Yo, I was on pioglitazone for a bit and the swelling was wild-felt like I was carrying water balloons for legs. Started daily weigh-ins and cut out processed junk, and boom, down 4 lbs in 10 days. No magic, just consistency. Also, elevating my feet while watching Netflix? Game changer.
Winni Victor
December 26, 2025 AT 16:59Ugh, another ‘just cut the salt’ lecture. Like I don’t already know that. But sure, let’s blame the patient for having kidneys that don’t magically turn into industrial desalination plants because Big Pharma decided to weaponize insulin sensitivity.
Lindsay Hensel
December 27, 2025 AT 20:22Thank you for this meticulously researched and compassionate overview. The distinction between fluid retention and adipose gain is critically undercommunicated in patient education materials. I urge all clinicians to share this with their patients-especially those navigating comorbidities.
Gary Hartung
December 28, 2025 AT 09:31...And yet, despite all the data, the FDA’s black box warning, the clinical guidelines, the meta-analyses... some doctors still prescribe TZDs like they’re handing out candy at a parade. It’s not just negligence-it’s institutional inertia wrapped in white coats.
Ben Harris
December 29, 2025 AT 08:40Jason Jasper
December 30, 2025 AT 15:42Interesting that SGLT2 inhibitors help with the edema. I wonder if that’s due to natriuresis overriding the TZD effect, or if there’s a downstream signaling interaction. Might be worth a quick literature dive.
Justin James
December 30, 2025 AT 18:49Did you know the pharmaceutical industry has been quietly funding studies that downplay TZD side effects since 2009? They know fluid retention leads to heart failure, but they also know that patients on these drugs stay on them longer-so they make more money. That’s why your doctor still pushes them. The FDA? They’re asleep at the wheel. Look up the 2015 internal emails from Takeda-there’s your smoking gun.
Rick Kimberly
January 1, 2026 AT 04:11Could you clarify whether the 45% reduction in edema risk with SGLT2 co-administration was observed in randomized controlled trials with intention-to-treat analysis? The magnitude of effect is compelling, but the clinical heterogeneity across studies warrants caution.
Terry Free
January 2, 2026 AT 01:35Wow. So let me get this straight. You want people to just ‘talk to their doctor’ instead of taking responsibility? Newsflash: doctors are overworked, underpaid, and don’t have time to play detective. If you’re gaining weight on TZDs, stop taking them. End of story. No one’s forcing you to be a guinea pig.
Sophie Stallkind
January 3, 2026 AT 21:32Thank you for emphasizing the importance of daily weight monitoring. In my clinical practice, this simple intervention has significantly reduced hospitalizations related to fluid overload. I encourage all patients to maintain a log-consistency is key.
Oluwatosin Ayodele
January 5, 2026 AT 07:13You all are missing the point. In Nigeria, we don’t even have access to SGLT2 inhibitors. We use metformin and TZDs because they’re cheap and available. Your fancy American solutions don’t work here. Stop lecturing people who are just trying to survive with what’s in the pharmacy.