Medication Switching Advisor
Find Your Safe Switching Strategy
Enter your current medication and new medication to calculate the best approach based on half-life, drug class, and potential interactions.
Recommended Strategy
Key Information
WARNING: Potential Danger
What to Expect
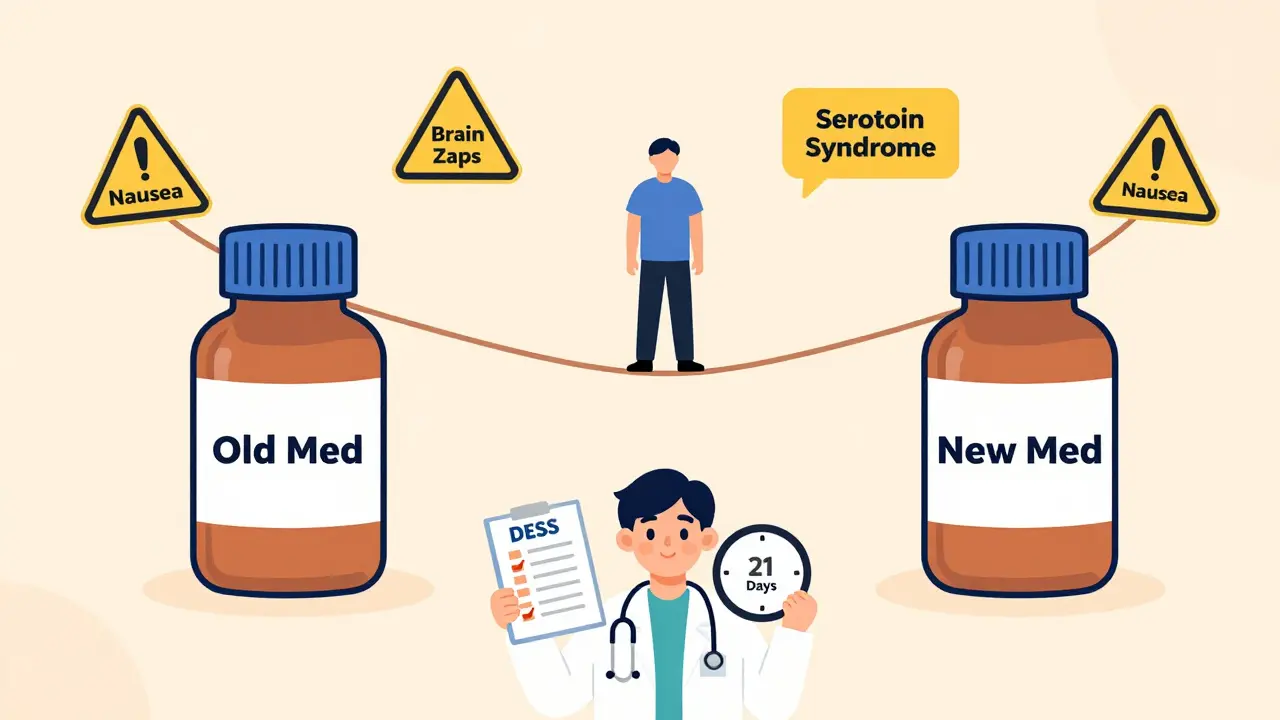
Why Medication Switching Can Go Wrong
Switching medications isn’t just changing one pill for another. It’s a delicate balancing act between stopping one drug safely and starting another without triggering a wave of side effects. For many people, especially those on antidepressants, anticonvulsants, or blood pressure meds, the transition feels like walking a tightrope. One wrong step - skipping a dose, rushing the process, or ignoring half-life differences - and you could end up with brain zaps, nausea, insomnia, or even serotonin syndrome.
It’s not rare. About 68% of people on antidepressants switch at least once in their first year of treatment. And nearly half of those experience some level of withdrawal or adverse reaction. The good news? Most of these problems are preventable. The key isn’t just what drug you switch to - it’s how you switch.
The Four Ways to Switch (And When to Use Each)
There are four main strategies for switching medications, each suited to different drugs and situations. Knowing which one applies to your case can make all the difference.
- Direct switch: Stop the old medication and start the new one the very next day. This works best when switching between drugs in the same class - like going from one SSRI to another (e.g., Lexapro to Zoloft). Studies show it’s 92% effective in these cases. But if you’re jumping from an SSRI to an SNRI like Cymbalta, this method triples your risk of serotonin syndrome.
- Conservative switch: Taper down the first drug slowly, then wait 3 to 5 half-lives before starting the new one. This is safest for drugs with long half-lives like fluoxetine (Prozac), which can stay in your system for over 25 days. It cuts side effects by 41%, but increases relapse risk by 22% because you’re off meds for so long.
- Moderate switch: A middle ground - taper the old drug, wait just 2 to 4 days, then start the new one. This works okay for most people, especially if the drug has a medium half-life. But it fails for short-acting drugs like venlafaxine (Effexor XR), where withdrawal hits fast and hard.
- Cross-taper: This is the most popular method among specialists. You slowly reduce the old drug while gradually increasing the new one over 7 to 14 days. It’s especially effective when switching between different classes - like from an SSRI to an SNRI or even from an MAOI (though MAOIs require extreme caution). About 63% of clinicians prefer this approach, and 82% of patients who used it reported minimal side effects.
Here’s the catch: cross-tapering isn’t always safe. Switching from an MAOI to an SSRI without a full 14-day washout can cause a dangerous spike in blood pressure. Always check for known drug interactions before starting.
Half-Life Matters More Than You Think
Not all drugs leave your body at the same speed. That’s called half-life - how long it takes for half the drug to be cleared from your system. This single number determines how long your washout period needs to be.
- Fluoxetine (Prozac): Half-life of 4-6 days. Washout needed: 25-30 days.
- Paroxetine (Paxil): Half-life of about 24 hours. Washout: 3-5 days.
- Venlafaxine (Effexor): Half-life of 5 hours. Withdrawal can start within 12 hours of missing a dose.
- Escitalopram (Lexapro): Half-life of 27-32 hours. Washout: 5-7 days.
Ignoring half-life is why so many people get hit with sudden symptoms. If you stop Paxil cold turkey, you might feel dizzy by day two. If you stop Prozac too soon after switching, you’re still carrying enough of it to cause dangerous interactions. Always check the half-life before planning your switch.
What You’ll Feel During a Switch - And What’s Normal
Some discomfort is expected. But not all symptoms are equal. Here’s what patients commonly report during transitions:
- Brain zaps: Electric-shock-like sensations in the head. Reported by 73% of SSRI switchers. Not dangerous, but deeply unsettling.
- Insomnia: Trouble sleeping. Affects 68% of people during withdrawal.
- Nausea and dizziness: Common with short-acting drugs like Effexor or Paxil.
- Anxiety or irritability: Often mistaken for relapse - but it’s usually withdrawal.
- Heart palpitations, sweating, or confusion: Red flags. Could mean serotonin syndrome.
Serotonin syndrome is rare - about 1 in 1,000 cases - but it’s life-threatening. Symptoms include high fever, rapid heart rate, muscle rigidity, and altered mental state. If you experience these, go to the ER immediately. It’s most likely when switching between drugs that both raise serotonin - like going from an SSRI to an SNRI without a proper washout.
How to Make the Switch Safer - Step by Step
- Get a full medication history. Your doctor needs to know every drug you’ve taken in the past year - including supplements and over-the-counter meds. Some herbal products like St. John’s Wort can interact dangerously with antidepressants.
- Check the half-life of both drugs. Use a reliable pharmacokinetic calculator or ask your pharmacist. Don’t guess.
- Use the Discontinuation Emergent Signs and Symptoms (DESS) checklist. This 10-item tool helps identify early withdrawal signs before they get worse. Your doctor should use it at every visit during the switch.
- Choose the right switching method. Cross-taper is safest for most transitions. Direct switch only if switching within the same class and both drugs have similar half-lives.
- Plan follow-ups. You’ll need at least three check-ins during the transition. The first should be within 3-5 days of starting the new drug.
- Have a backup plan. If symptoms flare up, your doctor might prescribe a short-term aid like hydroxyzine for anxiety or low-dose trazodone for sleep. Don’t push through severe symptoms.
Who’s at Higher Risk - And What to Do About It
Some people are more vulnerable during medication switches.
- People over 65: Experience 2.3 times more severe withdrawal symptoms. Slower metabolism means drugs stay longer, and side effects hit harder. Slower tapers are essential.
- Those with anxiety disorders: Withdrawal can mimic or worsen panic attacks. Cross-tapering and close monitoring are critical.
- Patients with multiple chronic conditions: More medications = more interaction risks. A pharmacist review is non-negotiable.
- People in rural areas: Limited access to specialists means many switch without proper guidance. If you’re in this group, ask your doctor about telehealth follow-ups or digital tools like the VA’s new switching decision aid.
There’s no one-size-fits-all, but the more you know about your body and your meds, the better your odds.
The Future of Switching: AI, Genetics, and Better Tools
Medication switching is getting smarter. In 2024, Google Health released an algorithm that predicts the best switching strategy for individual patients using real-world data from over a million people. It’s 83% accurate. The VA just integrated a similar tool into its electronic records, and it’s expected to prevent 12,500 adverse events each year.
Genetic testing is also becoming more common. Some clinics now test for CYP450 enzyme variants - genes that control how fast your body breaks down drugs. If you’re a slow metabolizer, you’ll need lower doses and longer tapers. One 2022 study showed a 33% improvement in outcomes when switches were guided by genetic data.
But tech isn’t a replacement for human judgment. A 2024 Lancet Psychiatry review found that experienced clinicians still outperformed AI in 61% of complex cases. The best approach? Use the tools, but trust your doctor’s experience - especially if you’ve had bad reactions before.
What to Do If Your Switch Goes Bad
Even with the best plan, things can go sideways. If you’re feeling worse after switching:
- Don’t stop the new drug suddenly. That can make things worse.
- Call your doctor. They might adjust the dose, slow the taper, or add a temporary support med.
- Track your symptoms. Use a simple journal: date, dose, symptoms, severity (1-10). This helps your doctor spot patterns.
- Reach out to patient communities. Reddit’s r/mentalhealth has thousands of firsthand accounts. You’re not alone.
Most people who stick with a structured plan end up feeling better than they did on their old medication. But it takes patience. The average transition takes 21 days. Don’t rush it.
Final Thought: It’s Not About the Drug - It’s About the Transition
Switching medications isn’t a failure. It’s often the next step in finding what works. The goal isn’t to avoid all side effects - it’s to manage them so they don’t derail your progress. With the right plan, the right timing, and the right support, you can switch safely, comfortably, and with confidence.
Can I switch medications on my own?
No. Switching medications without medical supervision can lead to serious side effects, including serotonin syndrome, seizures, or severe withdrawal. Always work with your doctor or pharmacist. Even if your old medication was prescribed by someone else, your current provider needs to approve any change.
How long do withdrawal symptoms last after switching?
Most withdrawal symptoms begin within 1-5 days after stopping the old drug and last 1-3 weeks. For drugs with long half-lives like fluoxetine, symptoms may appear later and linger for up to 6 weeks. Cross-tapering can reduce both onset and duration. If symptoms last longer than 4 weeks, talk to your doctor - it could be a sign of relapse or another issue.
Is cross-tapering always the best option?
Cross-tapering is the most effective method for switching between different drug classes - like from an SSRI to an SNRI. But it’s not ideal for everyone. It requires more frequent visits, careful dosing, and can be harder to manage if you’re on multiple medications. For simple switches within the same class (e.g., Lexapro to Zoloft), a direct switch may be safer and simpler. Your doctor will choose based on your specific drugs and history.
What if I miss a dose during the switch?
If you miss one dose of your old medication, take it as soon as you remember - unless it’s close to your next scheduled dose. If you miss a dose of the new medication, don’t double up. Just take your next dose at the regular time. If you miss multiple doses or are unsure, contact your doctor. Skipping doses increases the risk of withdrawal or destabilizing your condition.
Can I use over-the-counter supplements to ease withdrawal?
Some supplements like omega-3s or magnesium may help with general mood or sleep, but they don’t prevent withdrawal symptoms from prescription drugs. Avoid St. John’s Wort, 5-HTP, or tryptophan - they can raise serotonin levels dangerously when mixed with antidepressants. Always check with your doctor before taking anything new, even if it’s sold as "natural."


 Medications
Medications




Melissa Melville
February 2, 2026 AT 11:31Aditya Gupta
February 3, 2026 AT 04:31Deep Rank
February 3, 2026 AT 05:10Naresh L
February 3, 2026 AT 11:40Naomi Walsh
February 4, 2026 AT 08:44Bob Cohen
February 4, 2026 AT 11:44Ishmael brown
February 4, 2026 AT 21:50Nancy Nino
February 6, 2026 AT 11:13Angel Fitzpatrick
February 7, 2026 AT 19:57Nidhi Rajpara
February 8, 2026 AT 05:52