Every year, thousands of people accidentally crush, split, or chew their extended-release pills - not because they’re careless, but because they simply don’t know what the label means. If you’ve ever looked at a prescription bottle and seen ER, XR, or SR after the drug name and wondered what it meant, you’re not alone. These letters aren’t just jargon. They’re safety warnings in disguise.
What Extended-Release Really Means
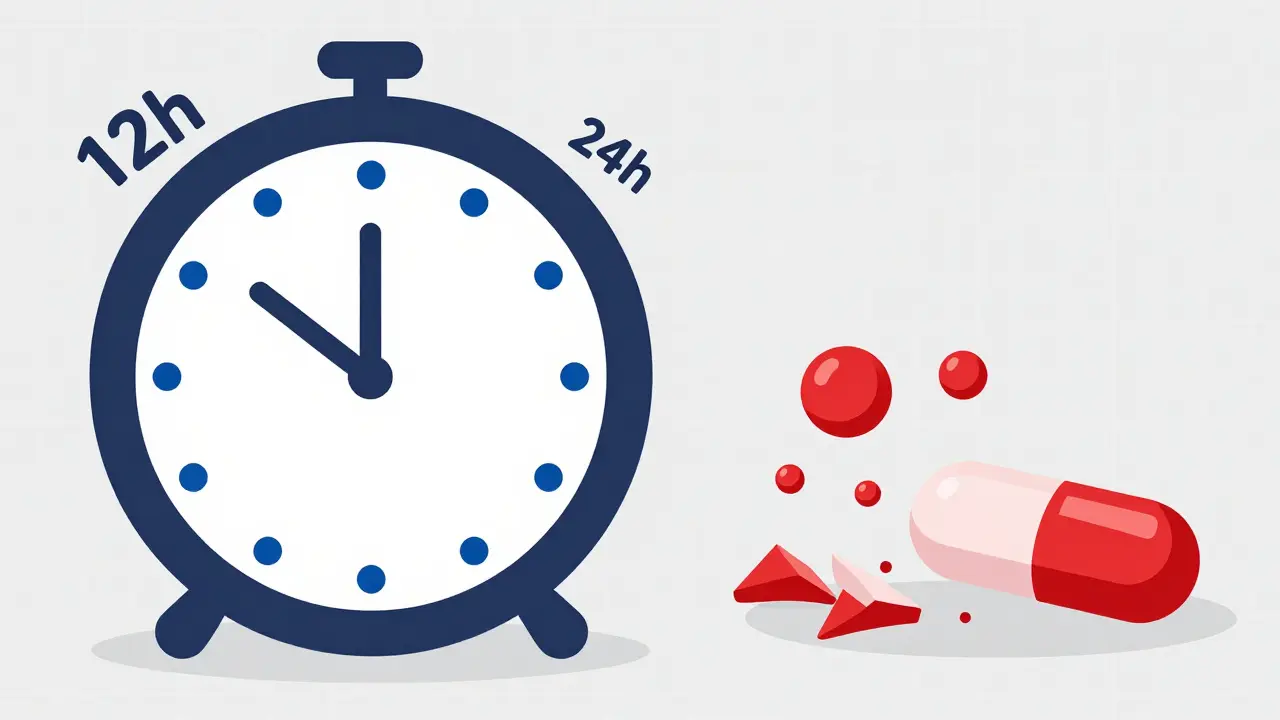
Extended-release medications are built to release medicine slowly over time - not all at once. That’s different from regular pills, which dump their full dose into your system right away. Think of it like this: a regular painkiller gives you a quick spike of relief, then fades fast. An extended-release version spreads that same amount of medicine out over 12 or 24 hours. That’s why you only need to take it once or twice a day instead of every four hours.The goal? Keep your blood levels steady. No highs, no lows. That’s better for your body, and it makes sticking to your schedule easier. But here’s the catch: if you break open that pill, you’re not just changing how it works - you’re risking a dangerous overdose.
Decoding the Letters on the Label
The most common suffixes you’ll see on extended-release meds are:- ER - Extended Release
- XR - eXtended Release
- SR - Sustained Release
- CR - Controlled Release
- CD - Continuous Delivery
These letters always come after the drug name. For example: metoprolol XR, oxycodone ER, or verapamil SR. Sometimes, you’ll also see a time frame: 24-hour extended release or 12-hour controlled release. That’s not extra fluff - it tells you exactly how long the medicine is designed to last.
But here’s where things get tricky. Not all ERs are the same. Two pills with the same label - say, “diltiazem ER” - can work completely differently inside your body. One might use a coating that dissolves slowly. Another might have tiny beads trapped in a gel matrix. Even if they’re both called ER, they’re not interchangeable. That’s why your pharmacist always asks if you’re switching brands.
The One Rule You Must Never Break
Never crush, split, chew, or open an extended-release pill unless your doctor or pharmacist says it’s okay.Why? Because you’re not just breaking the pill - you’re breaking the system. If you crush a 24-hour pill, you’re releasing all the medicine at once. That’s like taking four doses in one go. For opioids like oxycodone or stimulants like Adderall, that can cause breathing problems, heart rhythm issues, seizures, or even death.
The FDA has documented over 1,200 serious adverse events between 2018 and 2022 linked to people tampering with extended-release pills. One Reddit user shared a case where someone crushed 60mg of OxyContin and snorted it - they ended up in intensive care. That wasn’t a rare mistake. Pharmacists report seeing 2-3 such cases every month.
Even pills that look like they’re meant to be split - like some blood pressure meds - can be dangerous if they’re extended-release. Just because it’s scored doesn’t mean it’s safe to break. Always check the label.
Timing Matters More Than You Think
It’s not just about whether you take the pill - it’s when you take it.Some extended-release medications work best at night. Niaspan (niacin ER), for example, is usually taken at bedtime. Why? Because it causes flushing - a hot, red feeling across your face and chest. Taking it before bed means you’re asleep when it hits, and you wake up feeling fine.
Others, like Adderall XR, should be taken in the morning. If you take it at night, you won’t just be wide awake - you could be up for 36 hours. One user on Drugs.com wrote: “I took Adderall XR at night thinking it would last all day. I didn’t sleep for two days.” That’s not a myth. That’s a real side effect.
Some meds, like Gilenya for multiple sclerosis, are designed to be taken once daily - and missing a dose or taking it at the wrong time can throw off your whole treatment. Your body gets used to that steady rhythm. Break it, and your symptoms can flare up.
What to Look for on the Label
FDA rules require all OTC and prescription labels to include four key sections for extended-release meds:- Uses - What the medicine treats.
- Warnings - This is where you’ll see “Do not crush, split, or chew.” It’s often in bold or red.
- Directions - Exact timing: “Take once daily in the morning,” or “Take at bedtime.”
- Inactive Ingredients - Lists fillers and coatings. Not important for most people, but if you have allergies, this matters.
Some newer labels have QR codes. Scan them with your phone - they link to short videos showing exactly how to take the pill. If your bottle has one, use it. It’s clearer than reading 10 lines of tiny print.
Common Mistakes People Make
- Thinking “extended release” means “longer-lasting effect” - It does, but that’s not the whole story. The key is how it releases, not just how long it lasts.
- Assuming all ER versions of the same drug are the same - Three different brands of diltiazem ER exist. None can be swapped without checking with your doctor.
- Skipping the Medication Guide - If your pill comes with a paper guide, read it. It’s not optional. It’s required by law for high-risk meds like opioids and certain heart drugs.
- Not asking your pharmacist - If you’re unsure, ask. Say: “Is this one safe to split?” or “Should I take this with food?”
A 2022 FDA study found that 42% of adults over 65 misunderstood the “do not crush” warning. They thought it just meant “don’t break it into pieces” - not that crushing it could kill them.

What’s Changing in 2026
Starting January 2024, the FDA began requiring all new extended-release labels to have high-contrast, bold “DO NOT CRUSH” warnings. That’s a big step. But the real change is happening behind the scenes.Electronic health records now require pharmacists to write “24-hour extended release” instead of just “ER” in digital prescriptions. That cuts down on mix-ups. And by 2027, nearly half of all new drugs will use extended-release tech - meaning this isn’t going away. It’s becoming the norm.
Some companies are even testing pills that last 48 to 72 hours using new stomach-retention systems. That’s great for adherence - but it also means the labels will get even more complex. Knowing how to read them now will save you trouble later.
What to Do If You’re Still Unsure
If you’re confused - stop. Don’t guess.- Call your pharmacist. They have 10 minutes to walk you through it.
- Use the “teach-back” method: After they explain, say, “So if I take this at night, I won’t feel dizzy in the morning - is that right?”
- Keep a small note in your wallet or phone: “My ER pill: [Drug Name] - Do NOT crush - Take [time] daily.”
There’s no shame in asking. Millions of people do it every day. The real shame is waiting until something goes wrong.
Can I split an extended-release pill if it’s scored?
No, not unless the label or your doctor specifically says it’s safe. A scored line doesn’t mean the pill is designed to be split. Many extended-release pills have scored lines for manufacturing reasons, not for patient use. Breaking them can release the full dose at once, which can be dangerous. Always check the Medication Guide or ask your pharmacist.
Why do some extended-release pills cost more than regular ones?
Extended-release pills cost more because they use special technology - coatings, gels, or timed-release beads - that makes them harder and more expensive to produce. They also require more testing to prove they work safely over time. On average, they’re 20-35% more expensive than immediate-release versions. But they can save money long-term by reducing hospital visits from missed doses or side effects.
Can I take my extended-release pill with food?
It depends. Some extended-release pills need to be taken with food to help absorption - like certain cholesterol meds. Others should be taken on an empty stomach, or food might interfere with how slowly they release. Always follow the label. If it doesn’t say, ask your pharmacist. Never assume.
What should I do if I accidentally crush or chew an extended-release pill?
Call your doctor or poison control immediately. Don’t wait for symptoms. Even if you feel fine, the full dose may still be entering your system. For opioids or heart meds, this can be life-threatening. Keep the number for Poison Control (1-800-222-1222 in the U.S.) saved in your phone. In Australia, call 13 11 26.
Are generic extended-release pills as safe as brand-name ones?
They must meet the same FDA standards for effectiveness and safety. But they don’t always work the same way in your body. For example, there are three different 24-hour diltiazem generics - none are interchangeable. Always check with your pharmacist when switching brands. If you notice new side effects after switching, tell your doctor.



 Medications
Medications





Ian Cheung
January 11, 2026 AT 13:34Man I used to crush my XR pills thinking it’d work faster like a shot of espresso
Turns out I was just giving my heart a surprise party
Now I just read the label like it’s a survival manual
Life’s too short to guess with meds
Michael Marchio
January 12, 2026 AT 10:17It’s staggering how many people treat prescription labels like they’re optional reading material - like a menu at a diner they don’t feel like reading. The FDA didn’t write those warnings for fun. The 1,200+ adverse events aren’t statistics - they’re people who thought they knew better. And now they’re in the ICU because they didn’t pause for two seconds to ask, ‘What does ER even mean?’
It’s not just ignorance - it’s negligence dressed up as convenience.
Jake Kelly
January 13, 2026 AT 11:49I appreciate how clear this is. My dad took his blood pressure pill wrong for months because he thought the score mark meant he could split it. He didn’t realize it was ER until his doctor called him out. Now he keeps a sticky note on his pillbox. Simple fix, huge difference.
Ashlee Montgomery
January 14, 2026 AT 14:48There’s something deeply human about how we avoid reading instructions until something goes wrong
We assume familiarity equals understanding
But pills don’t care how long you’ve taken them
They only care if you followed the design
Maybe the real problem isn’t the label - it’s the belief that we already know
Ritwik Bose
January 16, 2026 AT 04:52Respectfully, this is one of the most important public health messages I’ve read in years. In India, many patients split pills out of cost concerns or because pharmacists don’t always explain properly. I will share this with my family and community. Thank you for writing with such clarity and care.
🙏
Paul Bear
January 17, 2026 AT 17:02Let’s be precise: ER, XR, SR, CR, CD - these are not interchangeable terms. They denote distinct pharmacokinetic profiles. Crushing an ER tablet with a matrix system versus a coated bead system produces different release kinetics - and different toxicity thresholds. The FDA’s 1,200-event database includes cases where patients ingested immediate-release equivalents of extended-release formulations - a bioequivalence fallacy with lethal consequences. If you don’t understand the difference between zero-order and first-order release kinetics, you shouldn’t be handling these meds without professional guidance. Period.
lisa Bajram
January 18, 2026 AT 10:40OMG I just realized I’ve been taking my niacin ER at 8am and feeling like I’m on fire by noon 😅
Now I’m switching to bedtime - thank you!!
Also - QR codes on labels?? YES PLEASE!! I’m 47 and still hate tiny print
Also also - my pharmacist just gave me a free pill organizer with the name of my meds printed on it - she’s a saint
Everyone go hug your pharmacist today 🤗
Jaqueline santos bau
January 18, 2026 AT 21:59Okay but have you heard about the guy who crushed his Adderall XR and ended up in the ER screaming at his cat? And then his wife posted it on TikTok and now it’s a meme? I mean… it’s funny until it’s your dad.
Also - why do they even put score lines on these pills if you’re not supposed to break them? That’s just cruel. Like a tease. A pharmaceutical tease.
Kunal Majumder
January 19, 2026 AT 01:13My uncle in Delhi takes his diltiazem ER and splits it because the brand is expensive. He says his doctor told him it’s fine. I showed him this post. He’s calling his doctor tomorrow. This kind of info saves lives. Thank you.
Aurora Memo
January 19, 2026 AT 07:09I’ve worked in pharmacy for 18 years. The most heartbreaking thing isn’t the overdose cases - it’s the people who say, ‘I didn’t know.’ They’re not lazy. They’re overwhelmed. The system doesn’t make it easy. This post? It’s the kind of thing we wish every patient would read before leaving the counter.
neeraj maor
January 20, 2026 AT 09:49Let me guess - this is all part of the pharmaceutical industry’s plan to make you dependent on expensive meds while hiding the truth that generics are just as dangerous. The FDA is in bed with Big Pharma. Why else would they allow ‘ER’ to mean five different things? Why not standardize? Why not force all manufacturers to use the same slow-release tech? Someone’s making billions off confusion. And you’re just reading the label like a good little consumer.
anthony martinez
January 21, 2026 AT 12:24So let me get this straight - you’re telling me I can’t just smash my OxyContin like a candy and call it a day?
Wow.
What a twist.
Jake Nunez
January 22, 2026 AT 12:45My cousin in Mexico told me they use the same ER pills there but the labels are in Spanish and sometimes the ‘DO NOT CRUSH’ is printed in gray, not red. People miss it. This post should be translated and shared everywhere. Knowledge is the only real prescription.
Christine Milne
January 24, 2026 AT 08:37While I appreciate the intent, this article is dangerously oversimplified. The FDA’s 2024 labeling changes are not a solution - they’re a Band-Aid. The real issue is that the U.S. healthcare system commodifies medication without investing in patient education. You don’t fix ignorance with bold fonts - you fix it with universal access to pharmacists. Until then, this is performative safety.