When your doctor says you need a pulmonary function test, it’s not just another box to check. These tests tell you what’s really going on inside your lungs-especially when you’re short of breath, coughing constantly, or just feel like you can’t catch your air anymore. Two of the most important tests are spirometry and DLCO. They’re simple, non-invasive, and packed with information. But if you don’t know how to read them, you’re missing half the story.
What Spirometry Actually Measures
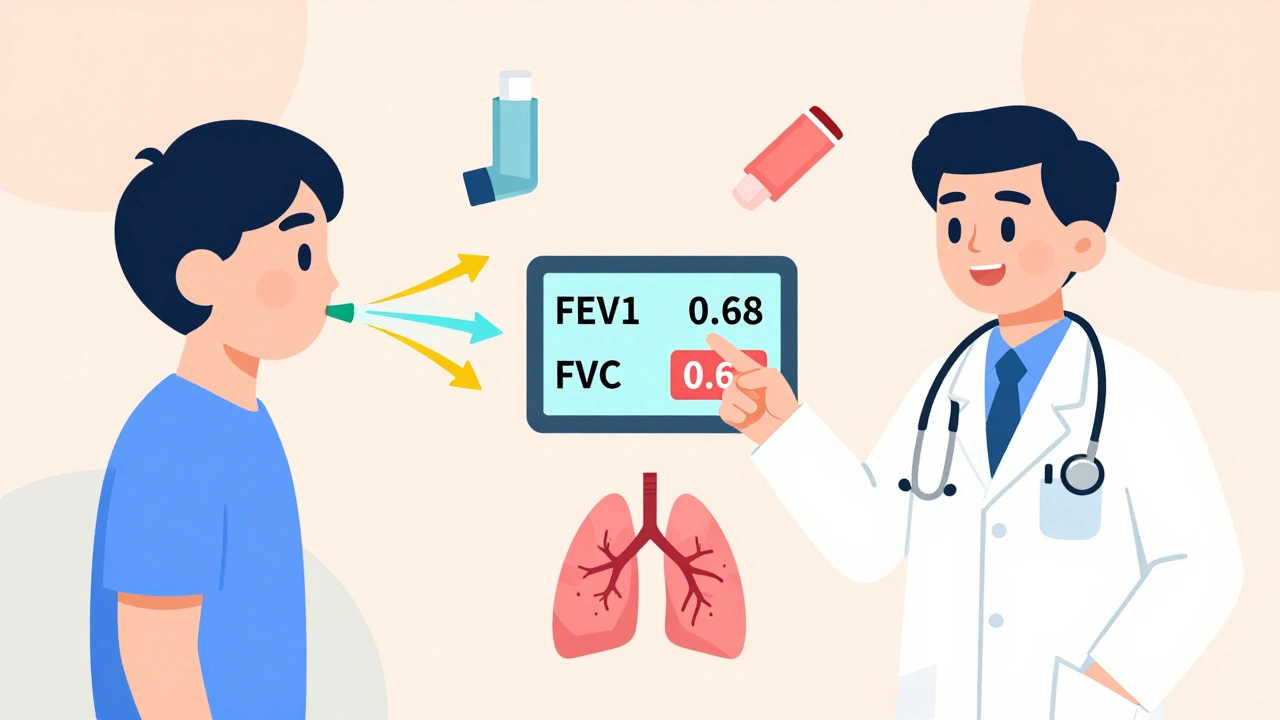
Spirometry is the first test most people get when lung problems are suspected. You breathe in as deep as you can, then blow out as hard and fast as you can into a tube connected to a machine. It sounds easy, but it’s not. You have to give it your all-no half-hearted attempts. The machine records two key numbers: FEV1 (how much air you can force out in the first second) and FVC (how much you can blow out total). Then it calculates the ratio: FEV1 divided by FVC. That ratio is everything. If your FEV1/FVC ratio is below 0.7, you likely have obstruction-think asthma, COPD, or emphysema. Your airways are narrowed, so air doesn’t flow out as quickly. But if the ratio is normal and your FVC is low? That’s restriction. Your lungs aren’t expanding fully. Could be scarring from past infections, obesity, or something like pulmonary fibrosis. Here’s the catch: spirometry alone can’t tell you why your lungs aren’t expanding. Is it because your chest wall is stiff? Or because your lung tissue itself is damaged? That’s where DLCO comes in.What DLCO Reveals That Spirometry Can’t
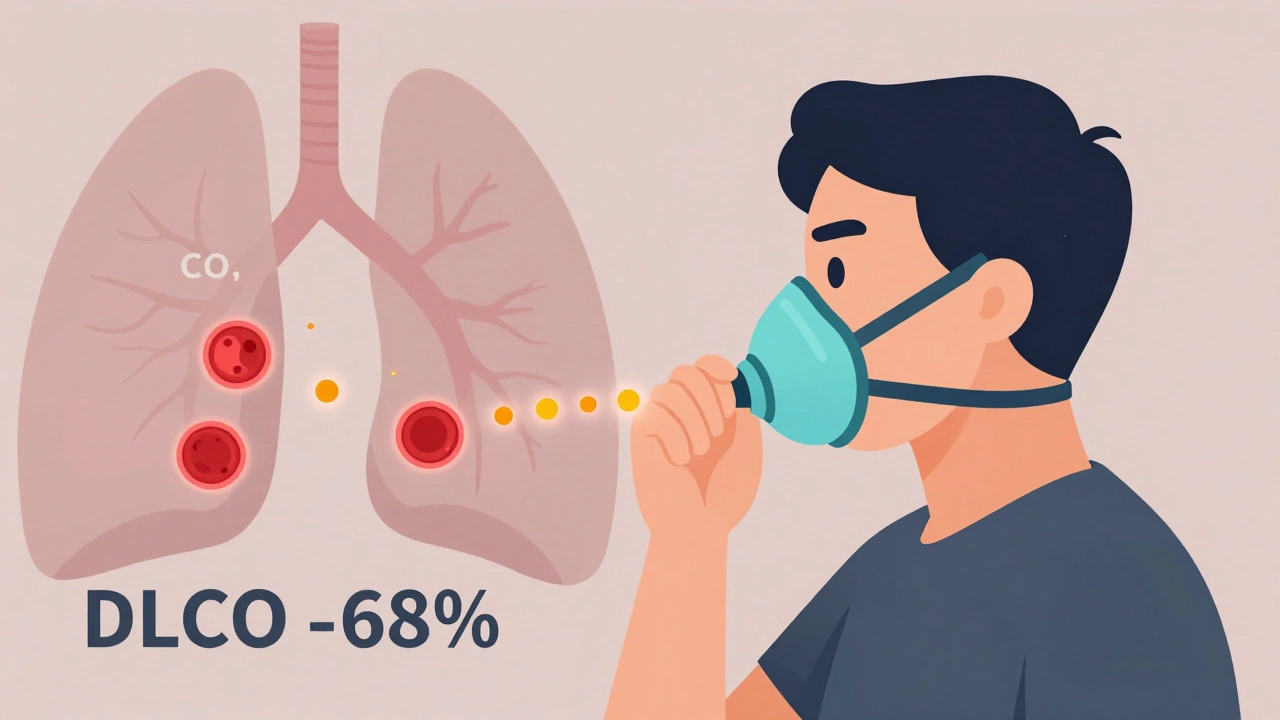
DLCO stands for diffusing capacity of the lung for carbon monoxide. Sounds complicated? It’s not. It measures how well oxygen moves from your lungs into your blood. That’s the whole point of having lungs-to get oxygen into your bloodstream. For this test, you inhale a tiny, harmless mix of gases-carbon monoxide, helium, oxygen-and hold your breath for exactly 10 seconds. Then you exhale. The machine compares how much CO you breathed in versus how much came out. The difference tells you how much was absorbed by your blood. Normal DLCO is between 75% and 140% of what’s predicted for your age, height, and sex. Below 75%? Something’s wrong with gas exchange. Above 140%? That’s unusual, but it can happen in conditions like polycythemia or early asthma attacks. The real power of DLCO is in the details. If you have low FVC (restriction) but normal DLCO, your lungs are probably physically restricted-maybe from obesity or scoliosis. The tissue itself is fine. But if your DLCO is low too? That’s a red flag for lung damage-interstitial fibrosis, emphysema, or pulmonary hypertension. The tiny air sacs (alveoli) or blood vessels are failing.Putting It Together: Real Patterns You’ll See
Here’s how these tests work together in real life:- Asthma: Spirometry may show obstruction (low FEV1/FVC), but DLCO is often normal-or even high during flare-ups. Why? Because your airways are inflamed, but your gas exchange is still working fine.
- Emphysema: FEV1/FVC is low (obstruction), and DLCO is almost always low. The walls between air sacs are destroyed. Less surface area = less oxygen transfer.
- Pulmonary fibrosis: Both FVC and DLCO are low. But DLCO drops first-sometimes months before spirometry shows anything. That’s why it’s so valuable for early detection.
- Pulmonary hypertension: Spirometry might look normal. But DLCO is low, and the ratio of FVC to DLCO is often above 1.6. This tells doctors the problem is in the blood vessels, not the lung tissue.
- Chronic pulmonary embolism: This one’s sneaky. Spirometry can be normal. But DLCO is low because clots block blood flow in the lungs. It’s one of the few conditions where DLCO is the main diagnostic clue.
Why DLCO Is Often Misunderstood
Even among doctors, DLCO gets overlooked. Why? Because it’s not as straightforward as spirometry. Several things can throw it off:- Anemia: Low hemoglobin means less oxygen-carrying capacity. That lowers DLCO-even if your lungs are perfectly healthy. A 1 g/dL drop in hemoglobin can reduce DLCO by about 1%.
- Smoking: Carbon monoxide from cigarettes sticks to hemoglobin, making it harder for the test to measure true uptake. Smokers often get falsely low DLCO readings.
- Age and height: DLCO naturally declines with age. Taller people have higher values. Reference numbers must be adjusted.
- Breath-hold timing: If you hold your breath for 8 seconds instead of 10, your DLCO will be wrong. That’s why proper technique matters.
When Doctors Order These Tests
You won’t get these tests unless there’s a reason. Common scenarios:- You’re short of breath and no one knows why.
- You have a chronic cough or wheeze that doesn’t respond to inhalers.
- You’re being evaluated for lung surgery.
- You have a connective tissue disease like scleroderma or lupus-both can quietly damage your lungs.
- You’re being monitored for pulmonary fibrosis. DLCO is tracked every 3-6 months to see if the disease is progressing.
What If Your Results Don’t Match Your Symptoms?
Sometimes you feel awful, but your tests look normal. That’s frustrating. But it doesn’t mean nothing’s wrong. If your spirometry and DLCO are both normal but you’re still struggling to breathe, the issue might be in your chest wall, diaphragm, or even your heart. Or it could be anxiety. But don’t assume that. Ask your doctor about bronchoprovocation testing (to check for asthma) or a six-minute walk test (to see how your oxygen drops with activity). And if your DLCO is low but your spirometry is fine? That’s a red flag for early disease. Don’t wait. Follow up with a high-resolution CT scan. You might have early interstitial lung disease-something that’s treatable if caught early.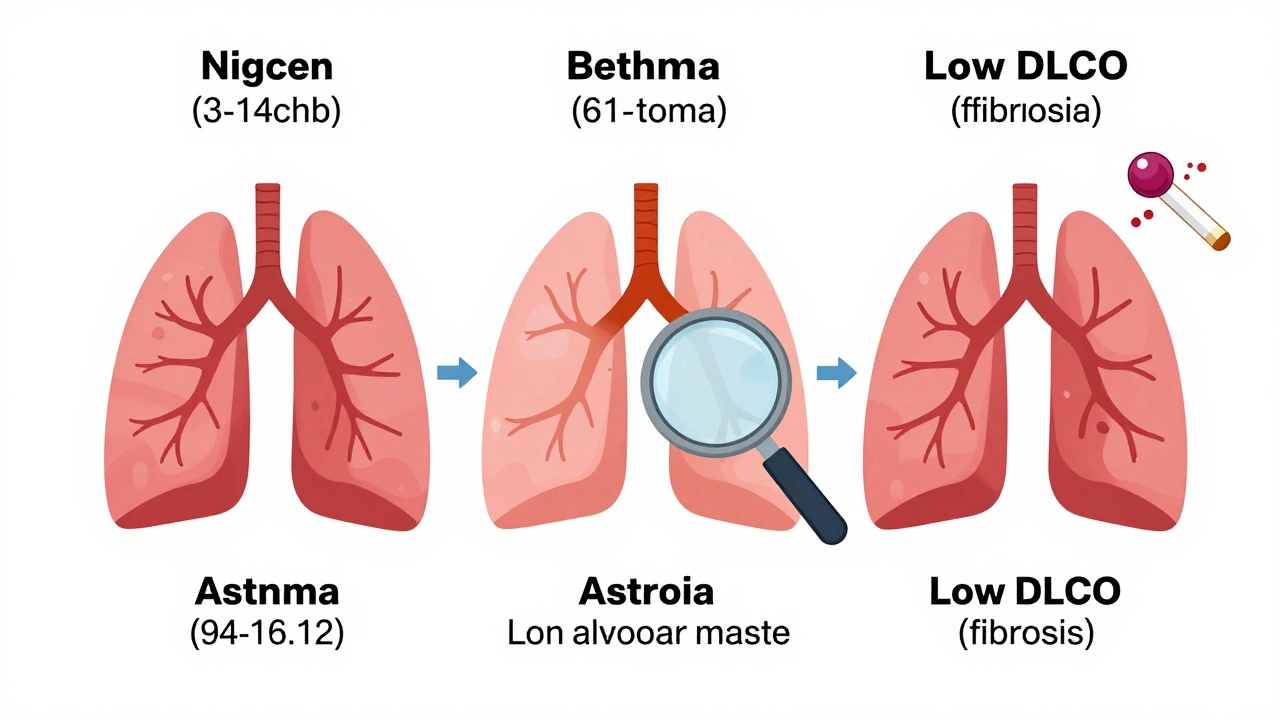
What to Do After Your Test
Don’t just get your results and walk away. Ask:- What’s my FEV1/FVC ratio? Is it below 0.7?
- Is my DLCO below 75%? If so, what could be causing it?
- Was my hemoglobin checked? Can I see that number?
- Do I need a CT scan or further testing?
Future of Lung Testing
Artificial intelligence is starting to help interpret these tests. A 2023 study from Mayo Clinic showed AI could predict pulmonary hypertension from DLCO patterns with 88% accuracy. That’s not replacing doctors-it’s helping them see patterns faster. And the tests themselves? They’re not going anywhere. Medicare still pays $85-$110 for DLCO. Hospitals still use them. And for good reason: they’re cheap, safe, and more informative than most blood tests. The bottom line? Spirometry tells you if air is flowing. DLCO tells you if oxygen is getting through. Together, they give you the full picture. Ignore one, and you’re flying blind.What does a low DLCO mean?
A low DLCO means your lungs aren’t transferring oxygen into your blood as well as they should. This can happen with emphysema, pulmonary fibrosis, pulmonary hypertension, chronic pulmonary embolism, or anemia. It’s not a diagnosis by itself-it’s a clue that points to damage in the tiny air sacs or blood vessels of the lungs.
Can you have normal spirometry but still have lung disease?
Yes. Many early lung diseases, like pulmonary fibrosis or chronic pulmonary embolism, show up first as a low DLCO-even when FEV1 and FVC are normal. That’s why DLCO is so important. It catches problems spirometry misses.
Why is hemoglobin important for DLCO?
Hemoglobin carries oxygen in your blood. If your hemoglobin is low (anemia), your DLCO will be artificially low-even if your lungs are healthy. Every DLCO result should be interpreted with your hemoglobin level. A drop of 1 g/dL in hemoglobin can lower DLCO by about 1%.
Is DLCO testing painful?
No. It’s completely painless. You just breathe in a harmless gas mixture, hold your breath for 10 seconds, then breathe out. Some people feel lightheaded, but it’s rare. The test takes less than 5 minutes.
How often should DLCO be repeated?
For people with stable lung disease, once a year is typical. For progressive conditions like pulmonary fibrosis, it’s often checked every 3-6 months to track how fast the disease is advancing. If you’re on a new treatment, your doctor may check it sooner to see if it’s working.
Can smoking affect DLCO results?
Yes. Smoking raises carboxyhemoglobin levels in your blood, which interferes with the test. This can make your DLCO look lower than it really is. If you smoke, your doctor should know-because they may need to adjust the results or ask you to stop smoking for a few days before testing.
What’s the difference between restriction and obstruction?
Obstruction means your airways are narrowed-air flows out slowly. Think asthma or COPD. Restriction means your lungs can’t expand fully-like with scarring or obesity. Spirometry shows both, but DLCO helps tell you why: is it the lung tissue itself (low DLCO), or just the chest wall (normal DLCO)?
Can DLCO be normal in someone with emphysema?
Rarely. Emphysema destroys the air sacs, so DLCO is almost always low. But in very early stages, or if the damage is patchy, DLCO might still be in the normal range. That’s why a normal DLCO doesn’t rule out emphysema-CT scans are needed for confirmation.


 Medications
Medications


Steve Sullivan
December 9, 2025 AT 19:19Maria Elisha
December 11, 2025 AT 18:56Tejas Bubane
December 13, 2025 AT 08:46Lisa Whitesel
December 14, 2025 AT 01:06Andrea DeWinter
December 14, 2025 AT 22:23Sabrina Thurn
December 15, 2025 AT 01:16Angela R. Cartes
December 15, 2025 AT 06:40Andrea Beilstein
December 16, 2025 AT 07:51Larry Lieberman
December 17, 2025 AT 19:52precious amzy
December 18, 2025 AT 08:30Ajit Kumar Singh
December 19, 2025 AT 06:37iswarya bala
December 20, 2025 AT 07:09Simran Chettiar
December 21, 2025 AT 19:04om guru
December 23, 2025 AT 17:33Brianna Black
December 25, 2025 AT 13:13