When a generic drug company submits an application to the FDA, they’re not just asking for permission to sell a cheaper version of a brand-name medicine. They’re asking for approval that their product is therapeutically equivalent-same active ingredient, same strength, same dosage form, and same performance in the body. But for more than half of all applications, that approval doesn’t come on the first try. Instead, they get a deficiency letter.
A deficiency letter from the FDA isn’t a rejection. It’s a detailed roadmap of what’s missing, wrong, or unclear in your application. Think of it like a teacher returning a test with comments like, “Show your work” or “This calculation doesn’t match the formula.” Only in this case, the stakes are billions of dollars and patient access to life-saving medications.
What’s in a Deficiency Letter?
The FDA doesn’t send vague feedback. Each deficiency letter is a technical document, often 10 to 30 pages long, listing specific issues that must be fixed before approval. These aren’t minor typos or formatting errors. They’re substantive gaps in science, data, or manufacturing control that could affect the drug’s safety, effectiveness, or quality.
According to FDA data from 2024, over 70% of major deficiencies in Abbreviated New Drug Applications (ANDAs) fall into three buckets: drug substance (the active ingredient), drug product (the final pill or injection), and manufacturing processes. The rest are split between bioequivalence studies, labeling, and documentation.
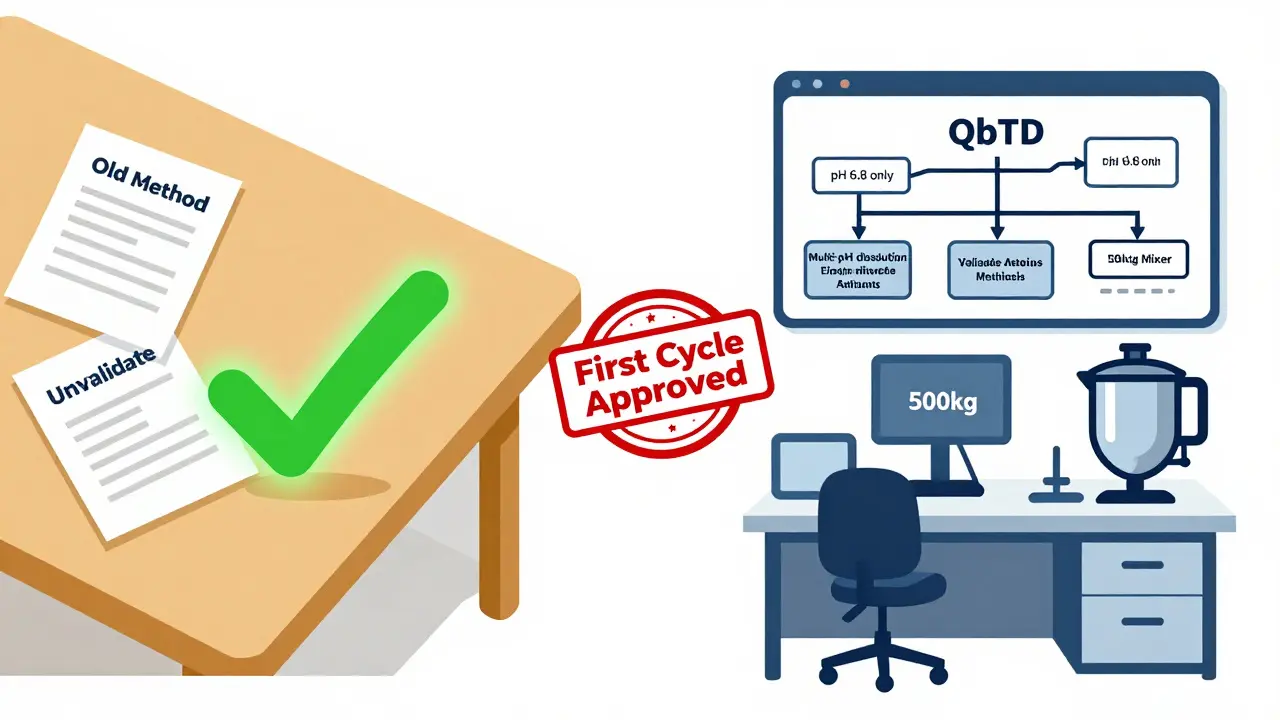
One of the most common issues? Dissolution testing. This is where the FDA checks whether the generic drug releases its active ingredient at the same rate and extent as the brand-name version. In 2023, 23.3% of ANDAs were flagged for problems here-either the test method was flawed, the specifications were too broad, or the apparatus used didn’t reflect real-world conditions in the human body. Many applicants still use outdated equipment like Apparatus 1 (basket) when Apparatus 2 (paddle) is required, or they test only at pH 6.8 when they need to show performance across pH 1.2, 4.5, and 6.8.
Top 5 Deficiency Categories (and Why They Happen)
Not all deficiencies are created equal. Some are easy to fix. Others can delay approval by over a year. Here are the five most frequent problems the FDA finds:
- Unqualified Impurities (20% of drug product deficiencies): Impurities are unintended chemicals in the drug. The FDA requires applicants to identify, quantify, and justify the safety of every impurity above 0.1%. Many companies skip or rush the toxicology studies needed for new impurities. One Teva regulatory manager reported these issues add 14 to 18 months to approval timelines because they require new animal studies.
- Drug Substance Sameness (19%): The generic drug’s active ingredient must be chemically and physically identical to the brand’s. For simple molecules, this is straightforward. But for peptides or complex APIs, it’s not enough to say “it’s the same.” You need data from circular dichroism, FTIR, and size-exclusion chromatography to prove the 3D structure, aggregation profile, and purity match. A 2023 study found nearly half of these failures came from academic-style development that never scaled to commercial production.
- Elemental Impurities (13%): ICH Q3D guidelines set strict limits for heavy metals like lead, cadmium, and mercury. Many applicants assume their raw materials are clean-but the FDA requires testing at every stage. One company got a deficiency because they used a catalyst in synthesis that introduced trace palladium, and they didn’t test the final product.
- Insufficient Analytical Method Validation (16.5%): The FDA doesn’t accept “we used the method from the brand’s application.” You must prove your method is accurate, precise, specific, and robust. That means running repeatability tests, spike recoveries, and stress testing under heat, light, and acidic conditions. A Reddit user in r/pharmaregulatory described how their dissolution method failed because they didn’t validate it under biorelevant media-only in plain water.
- Manufacturing Process Gaps: This isn’t just about paperwork. The FDA wants to see that your commercial-scale process matches the data you submitted. If you ran your bioequivalence batch on a 50kg mixer but your factory uses a 500kg mixer, that’s a red flag. You need to prove the process is scalable and controlled. In 2021, the FDA found that most failures for modified-release tablets came from multiple process gaps at once-filling, coating, and drying weren’t aligned.
Why Do Smart Companies Keep Getting Hit?
You’d think experienced teams would know the rules. But the data says otherwise.
Companies with fewer than 10 approved ANDAs face deficiency rates 22% higher than those with 50 or more. Why? It’s not lack of intelligence-it’s lack of institutional memory. Each deficiency letter is a lesson. If you don’t track them, you repeat them.
Another big issue? Misunderstanding the Bioequivalence Review Manual. The FDA says 30% of bioequivalence deficiencies come from applicants misinterpreting study design rules-especially for complex products like extended-release tablets or inhalers. One company submitted a crossover study with only 12 subjects because they thought that was enough. The FDA rejected it, saying 24 were required for high variability drugs.
And then there’s communication. A 2023 survey by the Association for Accessible Medicines found 78% of companies felt they didn’t get clear feedback from FDA reviewers. One applicant said they got a deficiency for “inadequate control strategy” for elemental impurities-but the letter didn’t say what control strategy would be acceptable. That’s not helpful. It’s frustrating. And it’s common.
How to Avoid Deficiency Letters
The good news? Most deficiencies are preventable.
Dr. David Rope, former head of the FDA’s Office of Generic Drugs, said in 2023 that 65% of major deficiencies could be avoided with better preparation. Here’s how:
- Request a pre-ANDA meeting. Companies that do this see deficiency rates 32% lower. You get direct feedback on your plan before spending millions on studies.
- Use Quality by Design (QbD) principles. Instead of testing the final product, design quality into the process. Map out critical quality attributes (CQAs) early. Define design spaces. This isn’t just trendy-it’s what the FDA wants.
- Validate methods like your reputation depends on it. Because it does. Don’t copy-paste methods from the brand’s label. Run your own validation studies. Include all relevant pH levels, temperatures, and stress conditions.
- Document everything. Applications with detailed development reports have 27% fewer deficiencies. The FDA isn’t just looking for data-they’re looking for logic. Show your thought process. Why did you choose this excipient? Why did you reject that manufacturing step? If you can’t explain it, they’ll assume it’s wrong.
- Track your own history. Keep a database of every deficiency letter your company received-even from past products. Look for patterns. If you’ve had three dissolution issues in five years, fix your testing protocol, not your application.
What’s Changing at the FDA?
The FDA knows deficiency letters are costly-for them and for patients. That’s why they’ve launched new initiatives.
In 2023, they started the First Cycle Generic Drug Approval Initiative, offering enhanced guidance and templates for the 10 most common deficiencies. In April 2025, they released sample responses showing exactly what acceptable answers look like-for dissolution, impurity control, and bioequivalence studies.
They’ve also created specialized review teams for complex products like peptides and modified-release formulations. Before, one reviewer might handle everything. Now, a peptide expert reviews peptides. That’s cut inconsistent feedback by 22%.
And by Q3 2026, the FDA plans to roll out AI-assisted pre-submission screening. The system will scan your application before you even hit “submit” and flag common errors: missing impurity profiles, wrong apparatus codes, unvalidated methods. Early tests show it could reduce preventable deficiencies by 35%.

The Real Cost of a Deficiency Letter
Behind every delay is money. Each additional review cycle costs generic companies an average of $1.2 million in lost time, retesting, and regulatory fees. For a low-revenue product under $10 million in annual sales, that’s a huge hit.
But here’s the kicker: high-revenue generics ($100M+ sales) have 18% fewer deficiencies. Why? They invest more in quality upfront. They hire experienced regulatory staff. They run pilot batches. They don’t treat the ANDA as a form to fill out-they treat it as a science project.
And then there’s the Competitive Generic Therapy (CGT) program. Products designated as CGT get priority review and extra guidance. Of those, 73% get approved on the first try-compared to the industry average of 52%. That’s not luck. That’s preparation.
By 2027, experts predict first-cycle approval rates could rise from 52% to 68%. That means more generic drugs hitting the market faster-cheaper, safer, and more accessible. But only if companies stop treating deficiency letters as punishments and start treating them as feedback.
Final Thought: It’s Not About Luck
Getting your ANDA approved isn’t about luck, timing, or who you know. It’s about rigor. It’s about understanding the science. It’s about doing the work before you submit.
The FDA doesn’t want to say no. They want to say yes-to safe, effective, affordable medicines. But they can’t say yes if the data isn’t there. And if you’re skipping steps, cutting corners, or assuming your method is good enough-you’re not helping patients. You’re just delaying them.
Fix the process. Don’t fix the application. That’s the difference between a deficiency letter and a green light.
What happens if I ignore a deficiency letter from the FDA?
Ignoring a deficiency letter means your application will not be approved. The FDA will not move forward until all listed issues are addressed. If you don’t respond within the required timeframe (usually 180 days), your application may be withdrawn. Even if you resubmit later, you’ll be treated as a new application and placed back at the front of the queue, losing all prior review progress.
Can I appeal a deficiency letter?
You can’t formally appeal a deficiency letter, but you can request a meeting with the FDA to discuss the findings. If you believe the deficiency is based on a misunderstanding, you can submit additional data, scientific literature, or a detailed rationale explaining why the issue doesn’t apply. The FDA reviews these responses on a case-by-case basis and may withdraw or modify the deficiency if your evidence is strong enough.
How long does it take to respond to a deficiency letter?
The FDA typically gives applicants 180 days to respond. However, complex issues-like new toxicology studies for impurities-can take 12 to 18 months to resolve. The response time depends on the nature of the deficiency. Simple documentation errors can be fixed in weeks. Manufacturing process changes or new bioequivalence studies can take over a year.
Do deficiency letters apply to all generic drugs?
Yes, deficiency letters apply to all Abbreviated New Drug Applications (ANDAs), regardless of the drug type. However, complex generics-like peptides, modified-release tablets, inhalers, and topical creams-are far more likely to receive them. These products require more complex testing and manufacturing controls, which increases the chance of gaps in the application. Simple immediate-release tablets have lower deficiency rates than complex formulations.
Is there a way to reduce the chance of getting a deficiency letter?
Yes. Requesting a pre-ANDA meeting with the FDA is the single most effective step. Companies that do this see deficiency rates 32% lower. Other proven strategies include using Quality by Design (QbD) principles, validating all analytical methods thoroughly, documenting development decisions clearly, and tracking past deficiencies to avoid repeating them. Investing in experienced regulatory staff also makes a big difference.
What’s the difference between a deficiency letter and a complete response letter?
There’s no difference. The FDA now uses the term “deficiency letter” for generic drug applications, but it’s the same thing as a complete response letter (CRL) used for brand-name drugs. Both list specific issues that must be resolved before approval. The term changed to reflect the fact that these letters are not final rejections-they’re requests for more information to complete the application.



 Medications
Medications


![Buy Generic Zovirax (Acyclovir) Online Cheap in the UK [2025]: Safe, Legal, and Fast](/uploads/2025/08/thumbnail-buy-generic-zovirax-acyclovir-online-cheap-in-the-uk-2025-safe-legal-and-fast.webp)
Jay Clarke
January 16, 2026 AT 21:30Let me tell you something-this whole FDA system is a rigged game. Companies spend millions just to get slapped with a deficiency letter because some bureaucrat in DC didn’t like the font size on page 17. It’s not about science anymore. It’s about power. And the real winners? Big pharma that lobbies to keep generics out. You think this is about safety? Nah. It’s about control.
Stacey Marsengill
January 18, 2026 AT 11:08I’ve seen this play out in my lab. One company spent 18 months fixing dissolution profiles just because they used a paddle instead of a basket. Meanwhile, the brand-name drug? They used a spoon and a coffee mug in their original study. The FDA doesn’t care about truth. They care about consistency. And consistency is just another word for tradition.
Aysha Siera
January 19, 2026 AT 13:02AI screening coming in 2026? Yeah right. That’s just the FDA’s way of outsourcing blame. The same people who wrote the guidelines 20 years ago are still in charge. They don’t want to fix the system-they want to automate the frustration. You think an algorithm can understand why a peptide’s 3D structure matters? Please. This is all theater. Patients are the ones paying the price.
rachel bellet
January 19, 2026 AT 19:28The notion that QbD reduces deficiencies by 32% is statistically insignificant without proper control variables. The cited correlation ignores confounding factors like organizational maturity, regulatory staffing density, and prior approval history. Moreover, the assumption that ‘documenting everything’ correlates with quality is a classic case of reification-treating procedural compliance as substantive scientific rigor. Until the FDA releases granular data on deficiency resolution timelines by company size, this entire narrative is anecdotal noise masquerading as evidence-based policy.
Pat Dean
January 21, 2026 AT 05:08Why are we even letting foreign labs handle this? Half these deficiencies come from Indian and Chinese manufacturers cutting corners. We used to make drugs here. Now we’re outsourcing quality control to people who don’t even speak English properly. If you can’t write a proper dissolution method in English, you shouldn’t be submitting to the FDA. This isn’t globalization-it’s national betrayal.
Selina Warren
January 22, 2026 AT 06:19Stop treating this like a paperwork game. This is life or death. Every delay in a generic drug approval means someone can’t afford their insulin. Every deficiency letter is a death sentence for someone on Medicaid. You think the FDA doesn’t know this? They do. But they’d rather hide behind jargon than fix the system. So here’s my call to action: if you work in pharma, stop playing nice. Demand transparency. Call out the delays. Stop accepting ‘we’ll fix it next time.’ Fix it now-or get out of the way.
Robert Davis
January 23, 2026 AT 02:41Interesting how the article mentions Teva and other big players but never names the small startups getting crushed by these letters. You know who gets ignored? The guy with a PhD and a garage lab trying to make a generic version of a $2000/month drug. He doesn’t have a regulatory team. He doesn’t have $1.2 million to waste. He just wants to help people. But the system doesn’t care about him. It only cares about the ones who can afford to play.
christian Espinola
January 24, 2026 AT 22:47There is a grammatical error on page 3: ‘They’re asking for approval that their product is therapeutic equivalent.’ Should be ‘therapeutically equivalent.’ Also, ‘Apparatus 1 (basket) when Apparatus 2 (paddle) is required’-this is technically accurate, but the FDA’s own guidance documents use ‘USP Apparatus 1’ and ‘USP Apparatus 2.’ Omission of ‘USP’ undermines credibility. These are the kinds of errors that trigger deficiencies.
Andrew Qu
January 26, 2026 AT 02:07Hey, if you’re reading this and you’re working on an ANDA-don’t panic. Deficiency letters aren’t the end. They’re a checklist. I’ve helped three small companies get approved after their first rejection. The key? Don’t argue. Don’t get defensive. Just answer each point, line by line, with data. Attach your validation reports. Show your method transfer logs. Be boring. Be thorough. The FDA loves boring. And if you’re stuck? Reach out to a consultant. It’s cheaper than a 14-month delay.
kenneth pillet
January 26, 2026 AT 13:45pre-ANDA meetings are gold. did one last year. got 3 minor notes. fixed em in 3 weeks. saved 8 months. no drama. just facts. if you’re spending millions on studies without talking to the FDA first… you’re just throwing money at the wall. talk to them. early. often. simple.
Danny Gray
January 26, 2026 AT 15:04Wait-so the FDA wants us to prove the drug works the same way… but they won’t tell us what ‘same’ means? That’s like asking a chef to replicate a dish but refusing to give them the recipe. And now they’re gonna use AI to scan for mistakes? Brilliant. Let’s automate the ambiguity. Next they’ll have a chatbot reply to deficiency letters with ‘Please clarify.’ That’s not innovation. That’s laziness dressed up as progress.
Zoe Brooks
January 28, 2026 AT 13:42Just want to say-this is actually really helpful. I’m a new regulatory specialist and I’ve been drowning in these letters. The breakdown of top 5 deficiencies? Lifesaver. And the part about tracking past letters? I’m starting a spreadsheet today. Thank you for writing this like a human. Not a robot. 💪
Kristin Dailey
January 29, 2026 AT 15:52Fix the process. Not the application. Done.