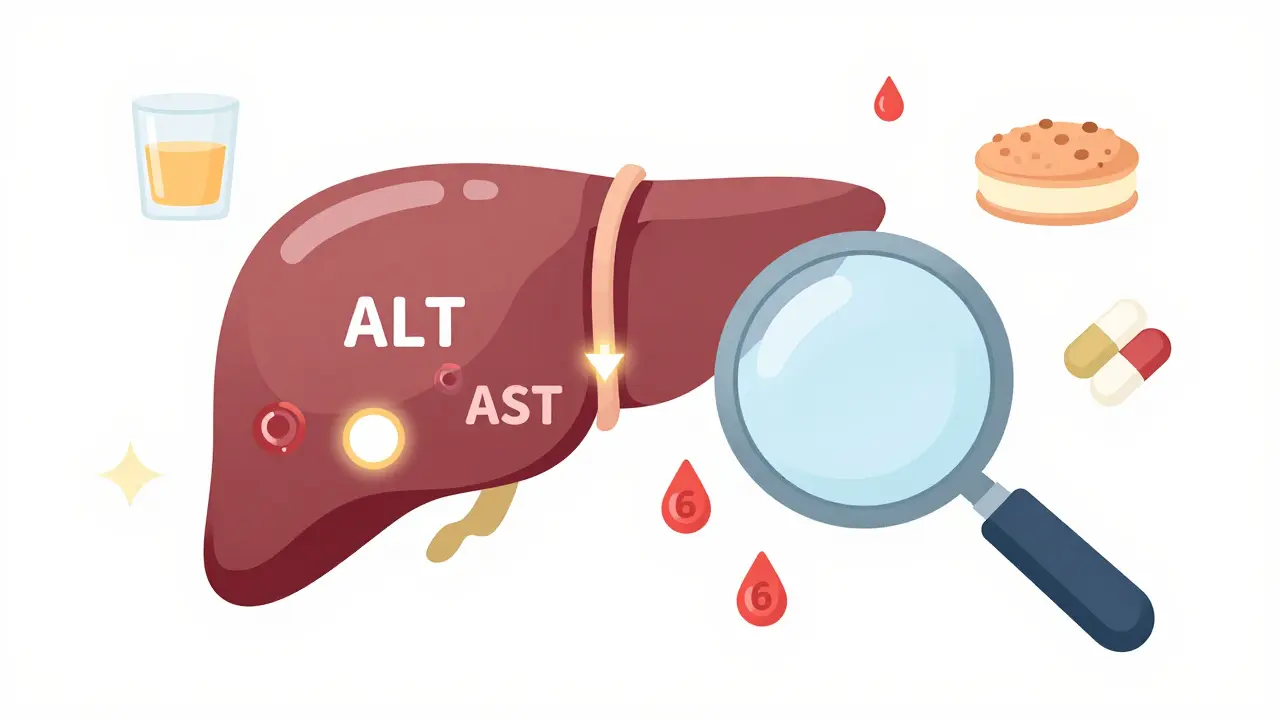
When your doctor orders liver function tests, they’re not checking how well your liver is working - they’re looking for signs it’s been damaged. The term liver function tests is actually a misnomer. These blood tests don’t measure bile production, detox capacity, or protein synthesis. Instead, they track leaked enzymes and waste products that spill into your bloodstream when liver cells are injured. Think of it like checking for smoke in a house - you’re not measuring heat, you’re detecting something’s wrong.
What’s Actually Measured in a Liver Panel?
A standard liver panel includes five key markers: ALT, AST, alkaline phosphatase (ALP), bilirubin, and albumin. Sometimes GGT and prothrombin time are added. Each tells a different part of the story.
- ALT (alanine aminotransferase): Mostly found in liver cells. When those cells break down, ALT leaks out. It’s the most specific marker for liver injury.
- AST (aspartate aminotransferase): Found in liver, heart, muscles, and kidneys. Less specific than ALT, but still useful when combined with other results.
- ALP (alkaline phosphatase): Elevated when bile flow is blocked - think gallstones, bile duct narrowing, or tumors pressing on ducts.
- Bilirubin: A yellow waste product from old red blood cells. When the liver can’t process or drain it, levels rise, causing jaundice.
- Albumin: A protein made by the liver. Low levels mean long-term damage - the liver is struggling to produce it.
Reference ranges vary by lab, but typical values in Australia are:
- ALT: 7-55 U/L (higher in men, higher in people with obesity)
- AST: 8-48 U/L
- ALP: 40-129 U/L
- Total bilirubin: 3-17 μmol/L
- Albumin: 35-50 g/L
Here’s the catch: normal doesn’t always mean healthy. About 10-15% of healthy people have ALT or AST slightly above normal - especially men, people with higher BMI, or those who exercise intensely. A value of 60 U/L isn’t a diagnosis. It’s a signal to look closer.
Patterns Matter More Than Numbers
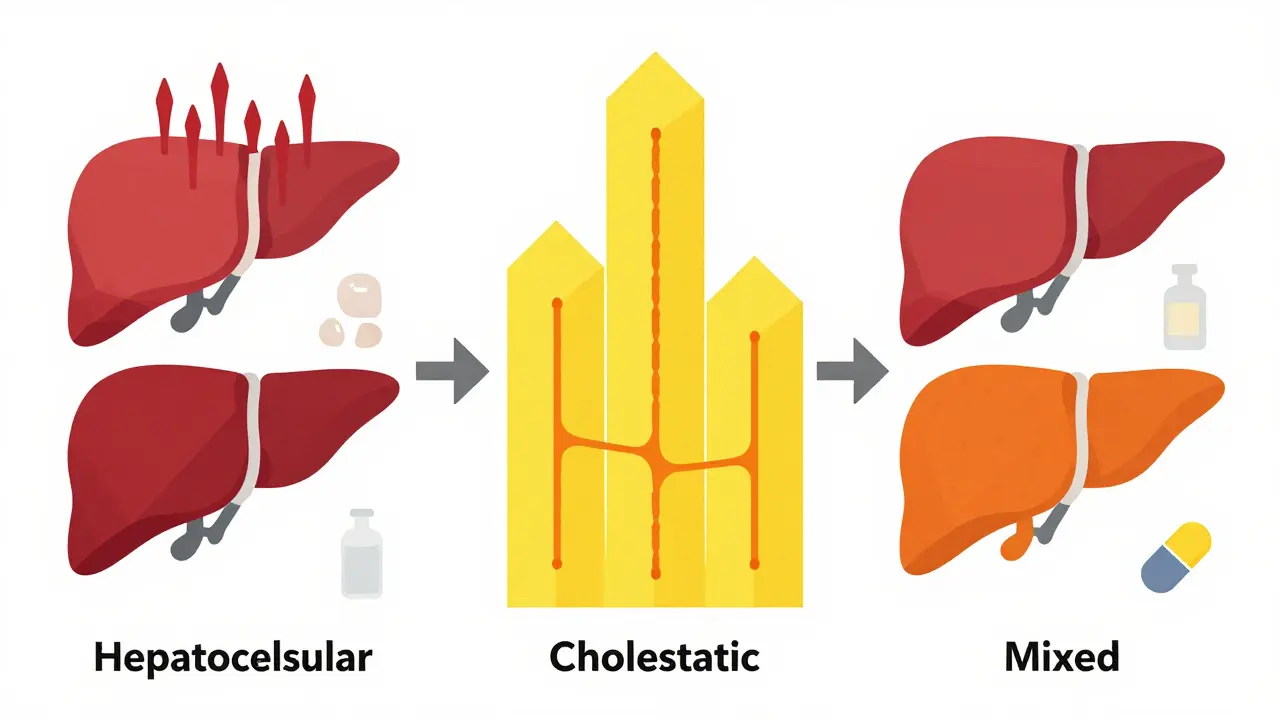
Doctors don’t look at each number in isolation. They look at the pattern. Three main patterns tell different stories.
1. Hepatocellular Pattern - Liver Cells Are Dying
This is the most common pattern. ALT and AST rise sharply, while ALP and bilirubin stay normal or only mildly elevated.
- ALT more than 10 times the upper limit? Likely acute viral hepatitis (like hepatitis A or B), paracetamol overdose, or ischemic injury.
- ALT 2-5 times normal, AST similar? Could be non-alcoholic fatty liver disease (now called MASLD), chronic hepatitis C, or drug reactions.
- AST twice as high as ALT? Strong red flag for alcohol-related damage. In alcoholic hepatitis, the AST:ALT ratio is often over 2.0.
Why does this happen? Alcohol damages liver cells directly, and in that process, it releases more AST than ALT. In contrast, fat buildup (MASLD) or viral hepatitis causes more ALT release because the injury targets the liver more specifically.
ALT has a half-life of about 47 hours. That means if you had a viral infection last week, ALT can still be high today. AST clears faster - around 24 hours. So if AST drops faster than ALT, it suggests the injury is healing.
2. Cholestatic Pattern - Bile Flow Is Blocked
This pattern shows ALP and bilirubin rising, while ALT and AST stay normal or only mildly elevated.
- ALP more than 3 times normal? Think gallstones, bile duct cancer, or primary biliary cholangitis.
- GGT also high? Confirms the source is the liver, not bones.
- ALP high but GGT normal? Could be bone disease - like Paget’s disease or healing fractures.
Bilirubin here is mostly conjugated - the kind the liver processes. If your skin or eyes turn yellow, it’s because the liver can’t get bile out. This isn’t about cell death. It’s about plumbing.
3. Mixed Pattern - Both Problems at Once
Many conditions don’t fit neatly. Drug-induced liver injury, autoimmune hepatitis, or advanced cirrhosis can show both cell damage and bile backup.
For example, someone on long-term statins might have ALT 150 U/L and ALP 200 U/L. That’s mixed. It’s not clear-cut. That’s when doctors look at symptoms, imaging, and other tests - not just numbers.
Bilirubin: More Than Just Jaundice
Bilirubin is broken into two types: unconjugated (before the liver processes it) and conjugated (after). Total bilirubin is the sum.
Unconjugated bilirubin rises in:
- Haemolytic anaemia (red blood cells breaking down too fast)
- Genetic conditions like Gilbert’s syndrome (harmless, affects 5-10% of people)
Conjugated bilirubin rises in:
- Blocked bile ducts
- Severe liver damage
- Medications like antibiotics or birth control pills
Isolated mild bilirubin elevation - say, 20 μmol/L - with normal liver enzymes? Probably Gilbert’s. No treatment needed. Just know it’s there.
Albumin and Prothrombin Time: The Real Function Tests
Here’s where most people get confused. ALT and AST show damage. Albumin and prothrombin time show how well the liver is still working.
Albumin takes 20 days to turn over. If your albumin is low (below 35 g/L), it means your liver has been struggling for months - maybe years. This is common in advanced cirrhosis or chronic alcohol use.
Prothrombin time (PT) measures how long it takes your blood to clot. The liver makes clotting factors. If PT is prolonged, your liver isn’t making enough. It’s an early sign of severe liver failure. Vitamin K deficiency (from poor diet or antibiotics) can also raise PT, so doctors check that too.
These aren’t “liver enzymes.” They’re signs of synthetic failure. If albumin is low and PT is high, the liver is in trouble - even if ALT and AST are normal.
What Causes Abnormal Results?
Here’s a quick guide to common causes:
- ALT high, AST normal or slightly high: Viral hepatitis, MASLD, drug reactions (like paracetamol, statins, antibiotics)
- AST higher than ALT: Alcohol, heart attack, muscle injury
- ALP and bilirubin high: Gallstones, bile duct cancer, primary biliary cholangitis
- All markers high: Severe hepatitis, drug toxicity, cirrhosis with bile backup
- Normal enzymes but low albumin: Chronic liver disease, malnutrition
And yes - muscle injury can raise AST. A heavy workout or crush injury can make AST spike to 1,000 U/L. That’s not your liver. That’s your biceps.
When Should You Worry?
Not every high number needs a scan or a specialist. Here’s the practical guide:
- ALT or AST 1-2 times normal: Monitor. Check weight, alcohol intake, medications. Repeat in 3-6 months. Most cases are harmless.
- ALT or AST 2-5 times normal: Investigate. Rule out fatty liver, hepatitis, medication side effects. Ultrasound often comes next.
- ALT or AST over 500 U/L: Urgent. Could be paracetamol overdose, acute viral hepatitis, or ischemic injury. Go to hospital.
- ALP >3x normal + jaundice: See a gastroenterologist. Need imaging - ultrasound or MRI.
- Low albumin + high PT: Likely advanced liver disease. Needs specialist care.
A 2021 study of over 12,000 patients found that combining LFT patterns with a simple score called FIB-4 (which uses age, platelets, ALT, AST) improved diagnosis of advanced liver scarring from 68% to 89%. That’s huge. Numbers alone aren’t enough. Context is everything.
What’s Next After a High Result?
If your LFTs are off, here’s what usually happens:
- Review your medications, supplements, and alcohol use. Even herbal teas can hurt the liver.
- Check for weight gain or diabetes. MASLD is the most common cause of elevated ALT in Australia today.
- Get an ultrasound. It’s non-invasive, cheap, and shows fat, fluid, or blockages.
- If still unclear, a FibroScan® may be done - it measures liver stiffness without a biopsy.
- Only if all else fails: viral hepatitis panel, autoimmune markers, or liver biopsy.
Don’t rush to a biopsy. Most cases are fatty liver or Gilbert’s. You don’t need a needle to know that.
What’s Changed in the Last Few Years?
In 2023, the term NAFLD (non-alcoholic fatty liver disease) was replaced with MASLD (Metabolic dysfunction-Associated Steatotic Liver Disease). Why? Because “non-alcoholic” was confusing. It didn’t capture the real cause: metabolic issues - insulin resistance, obesity, high triglycerides.
Also, new blood tests like the ELF test (Enhanced Liver Fibrosis) are being used in research. They measure three proteins that build up with scarring. In 2024, a Lancet study showed ELF combined with AST/ALT ratio detected advanced fibrosis with 92% accuracy. These aren’t routine yet - but they’re coming.
Bottom Line
Liver function tests aren’t a yes/no test. They’re a story. A pattern. A clue. A high ALT doesn’t mean you have cirrhosis. A normal AST doesn’t mean your liver is fine. You need to see the whole picture: your weight, your drinking, your meds, your symptoms, and how the numbers relate to each other.
If your result is slightly off - don’t panic. Most people with mild elevations never develop serious liver disease. But if your numbers are climbing, or you have symptoms like fatigue, dark urine, or swelling - act. Get checked. The liver doesn’t scream until it’s too late. But the tests? They whisper long before that.
Can alcohol cause high ALT and AST?
Yes. Alcohol damages liver cells, causing both ALT and AST to rise. But AST typically rises higher than ALT - often with an AST:ALT ratio greater than 2.0. This pattern is seen in about 90% of people with alcoholic hepatitis. Even moderate drinking over years can cause this.
Is a high bilirubin always a liver problem?
No. Unconjugated bilirubin can rise due to harmless conditions like Gilbert’s syndrome, which affects up to 10% of people. It often flares during fasting, illness, or stress. If ALT and AST are normal and you’re otherwise healthy, it’s likely not liver disease.
Can exercise raise liver enzymes?
Yes. Intense or unusual exercise can raise AST because it’s also found in muscle. A marathon or heavy weight session might push AST into the 300-500 U/L range. ALT usually stays normal. If your ALT is normal but AST is high, muscle injury is a likely cause - not liver damage.
Why is ALT more specific than AST for liver damage?
ALT is found almost entirely in liver cells. AST is also in heart, muscle, brain, and kidneys. So if AST is high but ALT is normal, the problem is likely not the liver - it could be a heart attack or muscle injury. ALT is the cleaner signal for liver-specific damage.
Should I get tested for hepatitis if my LFTs are high?
Yes, especially if ALT is over 100 U/L or you have risk factors like past blood transfusions, IV drug use, or unprotected sex. Hepatitis B and C often show no symptoms until liver damage is advanced. A simple blood test can rule them out - and if positive, treatment is highly effective.
Can fatty liver disease cause normal liver enzymes?
Yes. Up to 30% of people with fatty liver have normal ALT and AST levels, especially in early stages. That’s why ultrasound or FibroScan® is often needed - enzymes don’t always reflect fat buildup. Weight loss and exercise can reverse it, even if blood tests look fine.
What’s the best way to lower elevated liver enzymes?
Start with lifestyle: lose 5-10% of body weight if overweight, stop alcohol completely, avoid unnecessary medications (including herbal supplements), and control blood sugar if you’re diabetic. Exercise helps reduce liver fat. Most people see improvement in 3-6 months with these changes. No pills or supplements are proven to fix it - just real, consistent habits.


 Medications
Medications




Alex Flores Gomez
January 29, 2026 AT 01:38Bro this post is basically a medical textbook with a caffeine buzz. ALT and AST aren't just numbers-they're the liver's screaming into a pillow at 3am. And yeah, 'liver function tests' is a scam name. It's more like 'liver damage bingo.' I've seen people panic over 60 ALT like it's a death sentence. Nah. You ate pizza and did 100 burpees. Chill.
Frank Declemij
January 29, 2026 AT 04:14The distinction between hepatocellular and cholestatic patterns is critical for clinical decision-making. ALT specificity for hepatocellular injury versus ALP elevation indicating biliary obstruction provides a reliable framework for differential diagnosis. The AST:ALT ratio >2 is indeed a hallmark of alcoholic etiology, though muscle injury remains a common confounder.
DHARMAN CHELLANI
January 29, 2026 AT 15:06Liver tests? More like guesswork with a lab coat. You think ALT means liver? Nah. You lift weights? AST spikes. You're hangry? Bilirubin jumps. Doctors treat numbers like they're gods. Reality? Half the time it's just your body being a drama queen.
kabir das
January 29, 2026 AT 21:08Oh my GOD, I just found out my ALT was 68 last month... I'm so scared... I haven't slept since... I think I'm dying... I drank one beer last week... I'm sorry... I feel guilty... I'm going to cry now... Can someone please tell me I'm not going to die?!
Sheryl Dhlamini
January 31, 2026 AT 20:33I love how this breaks it down like a story instead of a textbook. I showed it to my cousin who's terrified of her liver results-and she actually smiled. Like, for the first time, she felt like she understood something medical. That’s rare. Thank you.
Ryan Pagan
February 2, 2026 AT 01:00Let’s be real-your liver is the ultimate silent ninja. It’ll take a beating from booze, sugar, and your ‘healthy’ protein shakes with 17 herbs, and still show up to work like nothing happened. Then BAM-suddenly it’s whispering in ALT and AST. By then? It’s been screaming for years. Don’t wait for jaundice. Cut the soda. Move your body. Sleep. That’s the real prescription. No pill in a bottle beats that.
Kristie Horst
February 2, 2026 AT 08:24It is truly remarkable how the medical community continues to use the term 'liver function tests' despite its inherent inaccuracy. One might argue that this misnomer perpetuates public misunderstanding regarding hepatic physiology. Furthermore, the inclusion of albumin and prothrombin time as indicators of synthetic function-while scientifically sound-is rarely emphasized in primary care settings, leading to significant diagnostic delays.
Andy Steenberge
February 2, 2026 AT 14:21Great breakdown. I’d add that Gilbert’s syndrome isn’t just harmless-it’s kind of cool. It’s like your liver has a chill personality. Fasts, stress, or a rough night? Bilirubin spikes. You’re fine. No meds. No panic. Just know you’re one of those 1 in 10 people who metabolize bilirubin like it’s a slow jazz song. Also-yes, muscle injury can spike AST. I once had a 420 AST after a 5K. My liver? Zero issues. My quads? Still crying.
Laia Freeman
February 4, 2026 AT 12:32OK BUT-did you know that your 'healthy' green juice with kale and wheatgrass? Yeah... that can spike ALT too. I went from 45 to 98 after 3 weeks of juice cleanses. My doc said, 'Stop drinking your plants.' I did. Two weeks later? Back to 48. So yeah. Even 'clean' stuff can mess with your liver. Don’t trust the wellness influencers. Trust science. And sleep.
rajaneesh s rajan
February 4, 2026 AT 13:27It's funny how we treat enzymes like oracles. We forget the liver is a survivor. It doesn't care if you're 'healthy' or 'unhealthy.' It just processes what you give it. Maybe the real question isn't 'why is my ALT high?' but 'what are you asking your liver to carry?' It's not a machine. It's a witness.
Megan Brooks
February 4, 2026 AT 20:10While the post provides a clinically accurate overview, I would respectfully suggest that the emphasis on lifestyle interventions be expanded to include socioeconomic factors. Access to fresh food, safe exercise spaces, and healthcare literacy significantly influence outcomes in MASLD and alcoholic liver disease. Numbers reflect biology, but context reflects justice.
Paul Adler
February 6, 2026 AT 03:22This is one of the clearest explanations I’ve seen. I’ve had patients come in terrified because their ALT was 62. I show them this post. They breathe again. The liver doesn’t fail overnight. It whispers. And most of the time? If you listen-really listen-it can heal. Thank you for translating science into humanity.