When you're diagnosed with tuberculosis, your doctor doesn't just pick one drug out of thin air. They build a treatment plan based on what works, what’s safe, and what your body can handle. Isoniazid has been the backbone of TB treatment for over 60 years. But it’s not the only option-and sometimes, it’s not even the best one for you.
Why Isoniazid Is Still Used
Isoniazid, often called INH, kills the bacteria that cause tuberculosis by stopping them from building their cell walls. It’s cheap, effective against active TB, and works well as a preventive shot for people exposed to TB but not yet sick. In fact, the CDC still recommends it as part of the first-line regimen for drug-susceptible TB.
But here’s the catch: Isoniazid alone won’t cure TB. If you take it by itself, the bacteria quickly learn to resist it. That’s why it’s always paired with other drugs. The standard six-month treatment includes isoniazid, rifampin, pyrazinamide, and ethambutol for the first two months, then just isoniazid and rifampin for the next four.
The Big Four: Isoniazid’s Main Partners
TB treatment isn’t about one hero drug-it’s about a team. Isoniazid’s most important teammates are:
- Rifampin: This drug stops TB bacteria from making RNA, which they need to multiply. It’s stronger than isoniazid at killing dormant bacteria and shortens treatment time when used together.
- Pyrazinamide: Works best in acidic environments, like inside immune cells where TB hides. It’s only used in the first two months because it can damage the liver if taken longer.
- Ethambutol: Prevents resistance by blocking bacterial cell wall synthesis. It’s often added at the start to cover unknown drug-resistant strains.
These four drugs form the backbone of what’s called the RIPE regimen-Rifampin, Isoniazid, Pyrazinamide, Ethambutol. Without isoniazid, this regimen falls apart. But what if you can’t take isoniazid at all?
When Isoniazid Isn’t an Option
Not everyone can tolerate isoniazid. Some people develop severe liver damage. Others have allergic reactions. A small number have nerve damage called peripheral neuropathy, especially if they’re malnourished, diabetic, or alcoholic. In these cases, doctors need alternatives.
The most common substitute is a regimen called Rifampin-Pyrazinamide-Ethambutol (RZE). It skips isoniazid entirely and relies on the other three drugs for longer-usually nine months instead of six. It’s less studied than the standard regimen, but studies from the WHO and CDC show it’s just as effective for drug-susceptible TB when taken correctly.
Another option is levofloxacin or moxifloxacin, which are fluoroquinolones. These aren’t first-line drugs, but they’re powerful. In 2023, the American Thoracic Society updated guidelines to include fluoroquinolones as part of alternative regimens for patients who can’t take isoniazid. They’re especially useful when liver problems make INH risky.
Comparing Side Effects
Every TB drug has risks. Here’s how isoniazid stacks up against its main alternatives:
| Drug | Common Side Effects | Severe Risks | Monitoring Required |
|---|---|---|---|
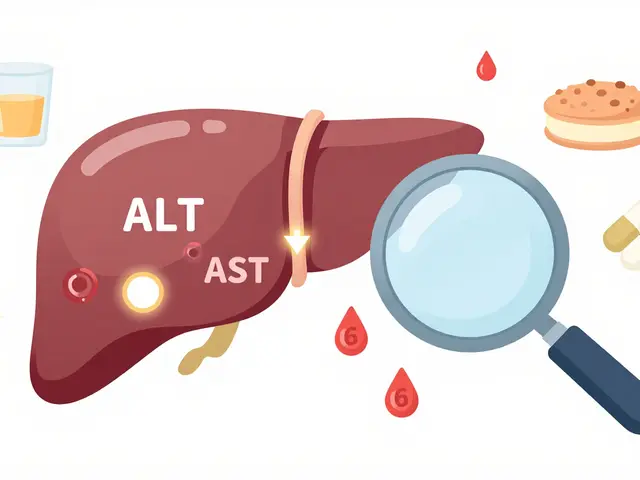
| Isoniazid | Nausea, dizziness, numbness in hands/feet | Liver damage (up to 1 in 100), nerve damage | Monthly liver enzyme tests |
| Rifampin | Orange urine, stomach upset | Liver damage, drug interactions (birth control, HIV meds) | Liver tests every 2-4 weeks |
| Pyrazinamide | Joint pain, loss of appetite | Severe liver injury, gout flare-ups | Liver tests, uric acid levels |
| Ethambutol | Blurred vision, color blindness | Permanent optic nerve damage | Eye exams before and during treatment |
| Levofloxacin | Nausea, headache, dizziness | Tendon rupture, nerve damage, heart rhythm issues | ECG monitoring, avoid in older adults |
Notice something? Isoniazid’s biggest risk is liver damage-but so is rifampin and pyrazinamide. Ethambutol’s vision risk is rare but permanent. Fluoroquinolones carry their own dangers, especially for older adults or people with kidney problems.
Drug Resistance Changes the Game
If your TB strain is resistant to isoniazid, then none of the standard regimens work. That’s when things get complicated. Multidrug-resistant TB (MDR-TB) means the bacteria don’t respond to at least isoniazid and rifampin.
In these cases, doctors use second-line drugs like bedaquiline, linezolid, or clofazimine. These aren’t alternatives to isoniazid-they’re alternatives to the whole first-line system. Treatment lasts 9-20 months, costs thousands of dollars, and has more side effects. But they save lives.
According to WHO data from 2024, about 3% of new TB cases worldwide are multidrug-resistant. In some regions, like Eastern Europe and parts of Asia, that number jumps to 15%. That’s why doctors test for drug resistance before starting treatment. You can’t treat TB blindly anymore.
What About Newer Options?
There’s been progress. In 2020, the FDA approved a new six-month all-oral regimen called BPaL-bedaquiline, pretomanid, and linezolid-for certain types of drug-resistant TB. It’s not for everyone, but for patients who can’t tolerate isoniazid and have resistant strains, it’s a breakthrough.
Another promising option is delamanid, which works similarly to bedaquiline. It’s not yet widely available in the U.S., but it’s used in Europe and parts of Africa. These drugs are expensive and reserved for cases where older drugs fail.
For people with latent TB (infected but not sick), isoniazid is still the go-to. But a newer alternative-rifapentine taken once a week with isoniazid for 3 months-is just as effective and easier to stick with. For those who can’t take isoniazid at all, a 4-month course of rifampin alone is now recommended by the CDC as a safe alternative.
Choosing the Right Path
There’s no single best drug. The right choice depends on:
- Your liver and kidney function
- Whether you’re taking other meds (like HIV drugs or birth control)
- If you have diabetes, alcohol use, or nerve conditions
- Whether your TB strain is resistant
- How well you can stick to daily pills for months
For most people with drug-susceptible TB, isoniazid remains essential. But if you can’t take it, you’re not out of options. Rifampin-based regimens, fluoroquinolones, and even newer drugs can do the job.
The key is testing early, communicating openly with your doctor, and not skipping doses. TB doesn’t care how good your plan is-it only cares if you take the pills.
Can I take isoniaiazid if I have liver disease?
No. Isoniazid can cause severe liver damage, especially in people with existing liver disease. If you have hepatitis, cirrhosis, or elevated liver enzymes, your doctor will avoid isoniazid and use alternatives like rifampin, ethambutol, or fluoroquinolones instead. Liver function tests are required before and during treatment.
Is there a shorter treatment than six months without isoniazid?
Yes. For drug-susceptible TB, a four-month regimen of rifampin and moxifloxacin is now approved by the CDC for patients who can’t take isoniazid. This option cuts treatment time in half and avoids INH-related risks. It’s not yet standard everywhere, but it’s gaining use in the U.S. and Europe.
What happens if I miss doses of my TB meds?
Missing doses is the #1 reason TB becomes drug-resistant. Even skipping a few days can let the strongest bacteria survive and multiply. That’s why directly observed therapy (DOT)-where a nurse watches you take each pill-is still used in many clinics. If you struggle to remember pills, ask about longer-acting alternatives or injectable options.
Are natural remedies effective against TB?
No. There is no scientific evidence that herbs, vitamins, or supplements can cure tuberculosis. TB is a bacterial infection that requires antibiotics. Relying on natural remedies delays real treatment and increases the risk of death or spreading drug-resistant TB to others.
Can I stop taking my TB meds once I feel better?
Absolutely not. TB bacteria can hide in your body for months, even after symptoms disappear. Stopping early lets those hidden bacteria wake up and come back stronger-and resistant to the drugs you took. You must finish the full course, no matter how good you feel.
Next Steps
If you’re starting TB treatment, ask your doctor: "Is isoniazid the right choice for me?" and "What are my alternatives if I can’t tolerate it?" Make sure you get tested for drug resistance before treatment begins. Keep a log of side effects. Tell your provider about every other medication you take-including supplements.
TB is curable. But only if the right drugs are used, and only if you take them every single day. The goal isn’t just to kill the bacteria-it’s to make sure they never come back.



 Medications
Medications




Margaret Wilson
November 20, 2025 AT 12:53So let me get this straight - we’re giving people a cocktail of chemicals that can blind them, wreck their livers, and rupture their tendons… and we call this ‘medicine’? 😅 I mean, TB is bad, but at this point I’d rather just hug a tree and hope the bacteria get bored.
Mary Follero
November 21, 2025 AT 10:31Actually, the 4-month rifampin-moxifloxacin regimen is a game-changer for people who can’t take INH - way fewer side effects and you’re done in half the time. I’ve seen patients thrive on it. Still need monitoring, but way more humane than the old 6-month grind. 🙌
william volcoff
November 21, 2025 AT 20:28Yeah, but let’s not pretend fluoroquinolones are harmless. Tendon rupture in someone over 60? That’s not a side effect - that’s a life-altering gamble. And don’t even get me started on how often people stop taking them because ‘they feel better.’
DOT isn’t just bureaucracy - it’s the difference between cure and a superbug outbreak.
Will Phillips
November 22, 2025 AT 20:22Arun Mohan
November 24, 2025 AT 06:53How quaint. In Delhi, we’ve been using bedaquiline off-label for years because INH was too toxic for our population - malnourished, diabetic, HIV-positive. You Westerners still cling to 1950s protocols like they’re sacred texts. The future is personalized regimens, not one-size-fits-all poison.
Jeff Moeller
November 26, 2025 AT 03:36Brad Samuels
November 26, 2025 AT 18:19I know someone who had to switch from INH to RZE after their liver enzymes went through the roof. Took nine months, but they’re clean now. It’s brutal, but not impossible. What helped was having a buddy system - one person checking in every day. Small things matter.
Tara Stelluti
November 27, 2025 AT 19:20So you’re telling me the CDC recommends a drug that can cause nerve damage… and then says ‘just get monthly liver tests’ like that’s enough? Like, what if I’m poor and can’t afford to miss work for a blood draw? What if I live in a food desert and can’t get the B6 supplements they say I need? This system is designed to fail people like me.
And then they act surprised when people stop taking it.
Tyrone Luton
November 28, 2025 AT 05:08It’s funny how we treat TB like a war - drugs as weapons, bacteria as enemies. But what if the real enemy is the belief that we can control nature with chemistry? Maybe we should be fixing housing, nutrition, access to care… instead of just handing out pills and calling it a day.
The bacteria aren’t the problem. The system is.
Freddy Lopez
November 30, 2025 AT 03:08There’s a quiet dignity in enduring a six-month regimen. It’s not glamorous. No one writes songs about it. But millions have walked this path - quietly, daily, alone. And we call it ‘treatment’ when it’s really an act of radical patience.
Maybe the real miracle isn’t the drug. It’s the human will to keep taking it.
Herbert Scheffknecht
December 1, 2025 AT 04:21Look - if you’re gonna take TB meds, you gotta treat it like a religion. Daily. No excuses. I know a guy who took his pills while on a hiking trip in the Rockies - wrapped them in foil, carried them in his boot. Said if he missed one, the bacteria would win. And he didn’t want to give them that satisfaction.
It’s not about being strong. It’s about being stubborn. And TB? It hates stubborn people.
Danielle Mazur
December 2, 2025 AT 12:54Did you know the WHO’s 2024 drug resistance data was partially funded by pharmaceutical lobbying groups? The numbers are manipulated to justify expensive new drugs like bedaquiline - which cost $20,000 a course - while basic INH remains underfunded. This isn’t science. It’s corporate strategy disguised as public health.