When patients move from hospital to home, mistakes in their medication lists can be deadly. A 2023 study found that nearly one in three patients leave the hospital with at least one error in their drug regimen. These aren’t just typos-they’re wrong doses, duplicate pills, or drugs that shouldn’t be taken together. And the people best trained to catch these errors? Pharmacists.
What Exactly Is a Pharmacist-Led Substitution Program?
A pharmacist-led substitution program is a structured service where pharmacists review a patient’s full medication list, spot dangerous gaps or overlaps, and swap out unsafe or unnecessary drugs for safer, more effective alternatives. It’s not just about switching brands. It’s about changing the entire treatment plan to fit the patient’s real-life needs. These programs started gaining traction after 2006, when The Joint Commission made medication reconciliation a national safety goal. But it wasn’t until 2010-2012 that hospitals realized pharmacists, not just doctors or nurses, were the right people to lead this work. Why? Because pharmacists know every drug’s side effects, interactions, and cost. They don’t just prescribe-they analyze. Today, 87% of U.S. academic medical centers and 63% of community hospitals run these programs. They’re not optional extras. They’re core to patient safety.How These Programs Actually Work in the Hospital
It starts the moment a patient walks in-or gets admitted. A medication history technician gathers the patient’s full drug list: prescriptions, over-the-counter pills, vitamins, herbal supplements, even what they took last week. This isn’t just asking, “What meds are you on?” It’s digging into details: “Did you skip your blood pressure pill because it made you dizzy? Did your daughter refill your diabetes meds without telling you?” Then, a pharmacist compares that list to what’s in the hospital’s electronic record. On average, they find 3.7 discrepancies per patient. One patient might be on five blood pressure drugs. Another might be taking two drugs that cause dangerous drowsiness together. A third might be on a proton pump inhibitor they don’t need anymore-increasing their risk of C. difficile infection. The pharmacist then makes substitutions. If a drug isn’t on the hospital’s formulary, they find a cheaper, equally effective alternative. If a drug is outdated or risky, they recommend stopping it-this is called deprescribing. In some programs, over half of all recommendations are for stopping drugs, not adding them. The whole process takes about 67 minutes per patient. But it’s worth it. Studies show these programs cut adverse drug events by 49%. That means fewer falls, fewer kidney failures, fewer ER visits.Why Pharmacists Beat Doctors and Nurses at This Job
Doctors are busy. Nurses are stretched thin. Pharmacists? Their whole job is drugs. A 2021 systematic review of 123 studies found that 89% of pharmacist-led programs reduced 30-day readmissions. Compare that to non-pharmacy-led efforts, where only 37% saw the same drop. The difference shows up most in high-risk groups: elderly patients on five or more medications, people with low health literacy, those with heart failure or diabetes. One trial-the OPTIMIST study-found that patients who got full pharmacist intervention were 38% less likely to be readmitted within 30 days. The number needed to treat? Just 12. That means for every 12 patients who get this service, one hospital readmission is prevented. And it’s not just about safety. It’s about cost. Each program saves hospitals $1,200 to $3,500 per patient by avoiding preventable admissions. Multiply that across thousands of patients, and you’re talking millions saved annually.The Hidden Hurdles: Physician Resistance and Time Crunches
Despite the evidence, these programs still face pushback. About 43% of academic medical centers report that doctors don’t always accept pharmacist recommendations. Why? Some feel it’s their job to decide. Others don’t trust the data. A few just don’t want to change their habits. Successful programs solve this with tech and teamwork. Electronic health records now auto-flag when a patient is on a non-formulary drug. Pharmacists get alerts. They send a quick note to the doctor: “Patient on warfarin and NSAID-high bleeding risk. Recommend switching to acetaminophen.” The note includes evidence. The doctor approves it 70% of the time. Time is the biggest barrier. Pharmacist-led programs need staffing. One pharmacist for every 3-4 technicians. In high-volume ERs, that means two full-time technicians Monday to Friday, plus part-time interns on weekends. Training takes time too-five eight-hour supervised shifts before a tech can work alone. But once trained, they hit 92.3% accuracy in collecting medication histories.
Deprescribing: The Quiet Revolution
One of the most powerful parts of these programs is stopping drugs-not adding them. Elderly patients often get stuck on medications they don’t need anymore. A proton pump inhibitor for heartburn? Maybe they stopped eating spicy food five years ago. Anticholinergics for overactive bladder? Those can cause confusion and falls. In the Beirut study, 52% of pharmacist recommendations were to stop a drug. That’s huge. And the results? Deprescribing anticholinergics led to a 41% drop in falls. Stopping unnecessary PPIs cut C. difficile infections by 29%. But here’s the catch: doctors only accept about 30% of deprescribing suggestions on their own. That’s why pharmacists need authority-not just advice-to make these changes.Where These Programs Are Growing Fastest
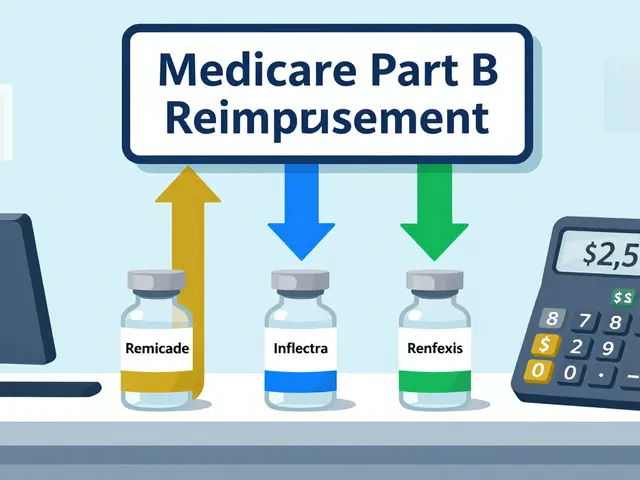
Hospitals were the first to adopt. Now, the wave is hitting post-acute care. By 2023, 42% of skilled nursing facilities had pharmacist-led deprescribing programs. That’s up from 18% in 2020. Why? Because nursing homes are full of patients on 10+ meds. Many are on drugs that were prescribed in the hospital and never reviewed again. The market is booming. The U.S. medication reconciliation services market hit $1.87 billion in 2022 and is growing at 14.3% per year. By 2027, it’s projected to hit $3.24 billion. Regulations are pushing this forward too. The 2022 Consolidated Appropriations Act now requires medication reconciliation for all Medicare Advantage patients. That’s 28.7 million people. CMS is also updating its rules to better reimburse pharmacists for this work.What’s Missing: Reimbursement and Rural Gaps
Here’s the ugly truth: even though these programs save money, they’re often underfunded. Only 32 states reimburse pharmacist-led substitution services through Medicaid. Medicare Part D covers some, but the paperwork is a nightmare. In community pharmacies, 68% of programs can’t cover their full costs because payers won’t pay. Rural areas are falling behind. Only 22% of critical access hospitals have full programs, compared to 89% in urban academic centers. Why? Pharmacist shortages. No one to run the service. The fix? Better payment models. Value-based care contracts are starting to include pharmacist outcomes. 63% of Accountable Care Organizations now tie bonuses to readmission rates-and they’re hiring pharmacists to hit those targets.
What’s Next: AI, Standardization, and Expanded Authority
New tools are making these programs faster and smarter. AI-powered apps now scan patient records and auto-suggest substitutions. One pilot at 14 hospitals cut data collection time by 35%. That means pharmacists spend less time typing and more time talking to patients. States are also expanding pharmacists’ legal authority. Twenty-seven state pharmacy associations are lobbying to let pharmacists initiate substitutions without doctor approval-especially for routine drugs like statins or blood pressure meds. The American Pharmacists Association, ASHP, and the American College of Clinical Pharmacy all agree: this isn’t experimental. It’s essential. They’ve given it Level A evidence-the highest possible rating.What Patients Should Know
If you’re going into the hospital or being discharged, ask: “Will a pharmacist review my medications?” If they say no, push back. This isn’t a luxury. It’s a safety net. Bring a list of everything you take-even gummies, tea bags, and supplements. Don’t assume they’ll know. Don’t trust memory. Write it down. And if you’re on more than five drugs, especially if you’re over 65, ask: “Is there anything here I can stop?” You might feel better without it.Final Takeaway
Pharmacist-led substitution programs aren’t about saving money. They’re about saving lives. They reduce deadly errors. They cut readmissions. They help people take fewer pills, not more. The data is clear. The experts agree. The systems are ready. What’s missing isn’t proof-it’s willpower. Hospitals need to fund these programs. States need to pay for them. Doctors need to trust them. The pharmacist isn’t just the person handing out pills. They’re the last line of defense before a mistake becomes a tragedy.What is a pharmacist-led substitution program?
A pharmacist-led substitution program is a clinical service where pharmacists review a patient’s full medication list, identify dangerous or unnecessary drugs, and replace them with safer, more effective alternatives. This includes switching to formulary-appropriate drugs, stopping inappropriate medications (deprescribing), and resolving discrepancies between what the patient takes and what’s documented in medical records.
Do these programs really reduce hospital readmissions?
Yes. Studies show pharmacist-led programs reduce 30-day readmissions by an average of 11%, with some high-risk groups seeing up to 22% reductions. A major trial called OPTIMIST found patients receiving full pharmacist intervention had a 38% lower risk of readmission compared to those who didn’t. The number needed to treat to prevent one readmission was just 12 patients.
Why are pharmacists better at this than doctors or nurses?
Pharmacists are trained specifically in drug interactions, side effects, dosing, and cost-effectiveness. While doctors focus on diagnosis and treatment plans, and nurses manage care delivery, pharmacists specialize in the full picture of medication use. This deep expertise allows them to spot hidden risks-like two drugs that cause dangerous drowsiness together-that others might miss.
What is deprescribing, and why is it important?
Deprescribing means safely stopping medications that are no longer needed, harmful, or inappropriate. It’s critical because many patients-especially older adults-take drugs they don’t need, like proton pump inhibitors for heartburn or anticholinergics for bladder control. These can cause confusion, falls, and infections. In pharmacist-led programs, over half of all recommendations involve stopping drugs, not adding them.
Why aren’t these programs in every hospital?
The biggest barriers are funding and staffing. These programs require trained pharmacists and technicians, and they take time-about 67 minutes per patient. Many hospitals can’t afford to pay for them because insurance reimbursement is inconsistent. Only 32 states fully reimburse these services through Medicaid, and Medicare Part D has complex paperwork. Rural hospitals also struggle due to pharmacist shortages.
Can pharmacists legally change my meds without a doctor’s approval?
In most cases, no-not yet. Pharmacists typically make recommendations to physicians. But 27 state pharmacy associations are pushing for laws that let pharmacists initiate substitutions for certain routine medications-like blood pressure or cholesterol drugs-without needing a doctor’s signature. These changes are slowly being adopted, especially in value-based care settings.
How can I make sure my pharmacist reviews my meds?
Ask directly: “Will a pharmacist review all my medications before I leave the hospital?” Bring a complete list of everything you take-including vitamins, supplements, and over-the-counter drugs. Don’t rely on memory. If your hospital doesn’t offer this service, ask why-and consider requesting it through patient advocacy channels. Your safety depends on it.


 Medications
Medications



Lawrence Armstrong
December 12, 2025 AT 23:28Just saw this at my mom’s hospital discharge last month. Pharmacist sat with us for 45 mins, crossed out 4 meds she didn’t need, swapped one for a generic that saved us $80/month. 😊 She even called her PCP to get it approved. No drama. Just good work. 🙌
sandeep sanigarapu
December 14, 2025 AT 17:59This is a very important initiative. Medication errors are a leading cause of preventable harm. Pharmacists possess specialized knowledge which is essential in this domain. The data presented is compelling and should be adopted universally.
Robert Webb
December 15, 2025 AT 10:08I’ve been in healthcare for 22 years, and I’ve seen this shift happen slowly but surely. I used to think doctors were the ones who knew everything about meds-until I watched a pharmacist catch a lethal interaction between a beta-blocker and an OTC cold med that the patient was taking because ‘it helped him sleep.’ That’s when it clicked. It’s not about hierarchy. It’s about who’s trained to see the whole picture. And honestly? The deprescribing part? That’s the quiet revolution nobody talks about. We’re overmedicating our elderly like they’re walking pharmacies. I had my own dad on a PPI for five years after a minor bout of heartburn-he hadn’t eaten spicy food since 1998. Stopped it, and his digestion improved overnight. No side effects. No rebound acid. Just… better. And that’s the thing-pharmacists don’t just fix mistakes. They undo decades of lazy prescribing. And yes, doctors resist. But when you show them the data-like the 38% readmission drop in OPTIMIST-it’s hard to argue. The real tragedy isn’t the resistance. It’s that so many hospitals still don’t have the staffing. One pharmacist for every three techs? That’s not luxury. That’s minimum viable safety. And if we’re not funding this, we’re just gambling with lives. And we’re losing.
Adam Everitt
December 15, 2025 AT 15:48pharmasists r the real unsung heros here. i mean, like, who else knows that mixing warfarin with ibuprofen is a one-way ticket to the er? docs are too busy signing papers. nurses got 12 patients. but the pharm? they got the book. and they use it. 🤓
wendy b
December 16, 2025 AT 01:21It’s fascinating how this profession has been systematically undervalued despite possessing the highest level of pharmaceutical expertise in the clinical ecosystem. The fact that physicians still hold veto power over pharmacists’ evidence-based recommendations speaks volumes about institutional inertia and professional ego. This isn’t healthcare-it’s a hierarchy masquerading as science.
Audrey Crothers
December 17, 2025 AT 14:27MY DAD WAS ALMOST KILLED BECAUSE NO ONE CHECKED HIS MEDS AFTER HIS STROKE!! 🥺 I had to beg the hospital to bring in a pharmacist. They said ‘we don’t have time.’ I said ‘then you don’t care enough.’ They finally did. Found THREE dangerous combos. One was a blood thinner he didn’t even know he was on. I cried. Like, ugly crying. Thank you for writing this. We need this EVERYWHERE.
Reshma Sinha
December 17, 2025 AT 16:10Medication reconciliation is a cornerstone of value-based care delivery. The ROI is demonstrable-reduced ADEs, lower readmission rates, enhanced patient adherence. Pharmacists as frontline clinical decision-makers in discharge workflows represent a paradigm shift in interprofessional collaboration. The 14.3% CAGR in this market segment is merely a reflection of systemic necessity.
Donna Anderson
December 19, 2025 AT 15:33my mom’s nurse said the pharmacist was just ‘giving advice’ but then she saw the list of meds they took off and was like ‘ohhhhh’ 😅 we saved like $200 a month and she stopped feeling like a zombie. i wish every hospital did this. why isn’t this automatic??
Rob Purvis
December 20, 2025 AT 20:51Just to clarify: the 67 minutes per patient? That’s not a luxury-it’s a baseline. And yes, the 92.3% accuracy rate for technicians after training? That’s insane. But here’s what no one says: if you’re a rural hospital with one part-time pharmacist and no techs, you’re not getting this done. And if you’re a Medicare Advantage patient in a state that doesn’t reimburse, your pharmacist can’t bill for it. So the system works… for the people who already have access. That’s not equity. That’s a privilege. And we’re calling it ‘best practice’? We need federal mandates. Not recommendations. Mandates.
Stacy Foster
December 22, 2025 AT 07:49THIS IS ALL A SCAM. Pharmacist-led programs? More like corporate cost-cutting disguised as safety. Who’s paying them? Big Pharma. They want you off expensive brand drugs and on generics they own. And deprescribing? That’s just cutting pills to save money-not because it’s safe. They’re killing patients with ‘simplification.’ You think they care about your grandma? They care about their stock price. And doctors who trust them? They’re being manipulated. Wake up.
Levi Cooper
December 23, 2025 AT 02:36Why are we letting foreigners and overqualified pharmacists run our healthcare? We used to have real doctors make decisions. Now we’ve got people with PhDs in pills telling our physicians what to do. This isn’t progress-it’s erosion of medical authority. And don’t get me started on how they’re replacing American jobs with tech and overseas-trained ‘experts.’ We need to take back our medicine.
Ashley Skipp
December 24, 2025 AT 07:19Everyone’s acting like this is new. It’s not. I worked in a hospital in 2008 and we had this. The doctors hated it. Said pharmacists were overstepping. Guess what? The readmission rate dropped 20%. They stopped complaining when the hospital got a bonus. Money talks. Always has.