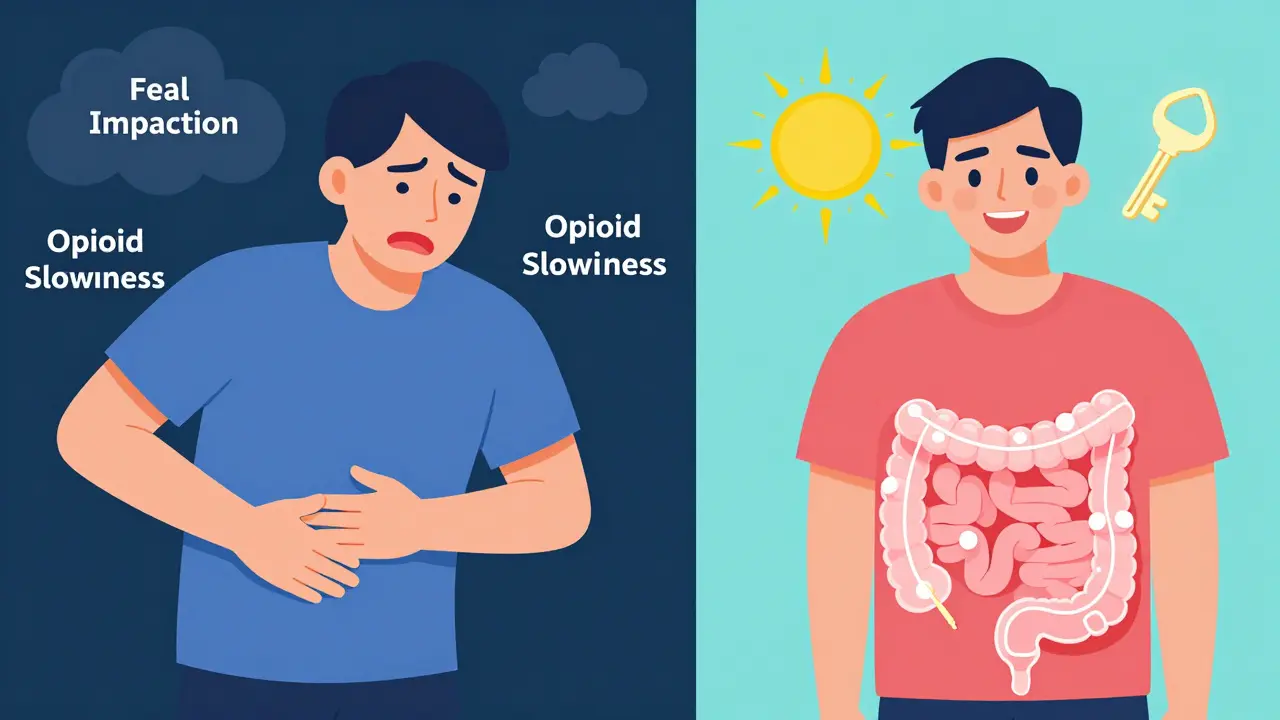
When you’re on long-term opioid pain medication, constipation isn’t just an inconvenience-it’s a silent barrier to your quality of life. Unlike nausea or drowsiness, which often fade after a few weeks, opioid-induced constipation (OIC) sticks around. It doesn’t get better on its own. And if left untreated, it can make you want to stop taking your pain meds altogether-even if they’re working perfectly for your pain.
Here’s the hard truth: up to 95% of people on chronic opioid therapy develop OIC. That’s not rare. It’s expected. Yet, only 15-30% of patients get proper prevention or treatment from their doctors. Why? Because many still think, "Just eat more fiber and drink more water," like it’s normal constipation. But that advice can actually make things worse.
Why Opioid Constipation Is Different
Opioids bind to receptors in your gut, slowing down everything. Your stomach empties slower. Your intestines stop moving. Your body pulls more water out of stool. The result? Hard, dry, painful bowel movements that feel like you’re trying to push a rock through a narrow pipe.
But here’s what most people don’t realize: this isn’t just "slow digestion." It’s a direct chemical effect. That’s why regular laxatives often fail. A 2023 review found that over-the-counter options like senna or bisacodyl only work for 25-50% of OIC patients. Even polyethylene glycol (Miralax), the go-to for general constipation, helps only about half the time.
And here’s the kicker: increasing fiber to 30g a day-a standard recommendation for constipation-isn’t safe for OIC. Fiber ferments in your gut, creating gas and bloating. With opioids already slowing things down, that trapped gas can lead to dangerous fecal impactions. The American Pain Society and Mayo Clinic both warn against high-fiber diets for OIC patients. In fact, 25-40% of people who follow this advice end up with worse symptoms.
First-Line Treatment: What Actually Works
Before you reach for another bottle of laxatives, start with the right tools. The first step is prevention-not reaction. If you’re starting opioids, your doctor should assess your bowel habits before you even take the first pill. Tools like the Bristol Stool Form Scale or the OIC Severity Scale help track changes.
For most people, the best first-line treatments are:
- Polyethylene glycol (PEG 3350) - 17-34 grams daily. It draws water into the colon without irritating the gut. It’s gentle, doesn’t cause cramping, and works better than stimulant laxatives for OIC.
- Bisacodyl - 5-15 mg daily. A stimulant laxative that triggers contractions. Use it only if PEG doesn’t help enough.
- Senna - 8.6-17.2 mg daily. Another stimulant. Can cause dependency if used long-term.
Take one of these daily, not just when you feel backed up. Waiting until you’re in pain means you’re already behind. Consistency beats urgency.
Most patients see improvement within 3-7 days. If not, don’t double the dose. Talk to your doctor. You may need something stronger.

When Over-the-Counter Isn’t Enough: Prescription Options
If laxatives aren’t cutting it-and for many, they don’t-it’s time to consider prescription drugs designed specifically for OIC. These are called peripherally acting μ-opioid receptor antagonists (PAMORAs). They block opioids in your gut without touching the pain relief in your brain.
Here are the three main options:
| Drug (Brand) | How It Works | Dosing | Onset | Common Side Effects | Best For |
|---|---|---|---|---|---|
| Methylnaltrexone (Relistor®) | Injectable PAMORA | 12 mg subcutaneous, as needed | 30 minutes to 4 hours | Injection site pain, dizziness, nausea | Palliative care, advanced illness |
| Naloxegol (Movantik®) | Oral PAMORA | 25 mg daily | 24-48 hours | Abdominal pain, diarrhea, headache | Chronic non-cancer pain |
| Naldemedine (Symcorza®) | Oral PAMORA | 0.2 mg daily | 24-48 hours | Abdominal pain, diarrhea, nausea | Adults with chronic pain, including elderly |
| Lubiprostone (Amitiza®) | Chloride channel activator | 24 mcg twice daily | 24-72 hours | Nausea (30%), diarrhea (15-20%) | Women (initial approval), though effective in men |
These drugs work differently than laxatives. They don’t irritate the gut. They don’t cause dependency. They just undo the opioid effect where it’s causing harm.
Response rates? Around 40-50% of patients have a meaningful improvement-double what you get with regular laxatives. But they’re expensive. Monthly costs range from $500 to $1,200. Insurance often requires you to try and fail on at least two laxatives first. That’s called step therapy. It’s frustrating, but common.
On patient forums, methylnaltrexone gets high marks for speed-many say relief comes in under 4 hours. But 47% report injection pain. Naldemedine has a better overall rating (6.8/10) and is easier to take daily. But 38% of users get abdominal pain. It’s a trade-off.
Why So Many People Still Go Untreated
Here’s the real problem: doctors don’t ask. Patients don’t bring it up. It’s embarrassing. You’re already dealing with chronic pain. Talking about bowel habits feels like adding insult to injury.
But here’s what patients don’t realize: untreated OIC is a major reason people stop taking opioids. One study found 30-40% of patients reduce or quit their pain meds-not because the pain came back, but because constipation became unbearable.
And it’s not just patients. A 2023 AMA survey found only 22-35% of community doctors use any standardized OIC assessment tool. Even though guidelines have existed since 2021, most primary care providers still don’t screen for it.
Meanwhile, nurses who use simplified protocols report 80% satisfaction. But doctors? Only 19% say they’re helpful. That gap matters.
What You Can Do Right Now
If you’re on opioids and struggling with constipation, here’s your action plan:
- Track your bowel habits - Use the Bristol Stool Scale (1 = hard lumps, 7 = watery). Aim for type 3-4.
- Start PEG daily - Not when you’re backed up. Every day. 17g minimum. Increase to 34g if needed.
- Stop high-fiber diets - No more bran cereal, psyllium husk, or extra veggies. They can trap gas and make impactions worse.
- Hydrate - Drink 2-3 liters of water daily. Fiber doesn’t help without water, and neither does PEG.
- Ask your doctor about PAMORAs - If you’ve tried PEG and stimulants for 2 weeks with no relief, it’s time to talk about Movantik or Symcorza.
- Check your insurance - Ask if you need to fail two laxatives first. If yes, get documentation of your trials.
Don’t wait until you’re in agony. Don’t assume your doctor will bring it up. Be the one to say: "I’m having constant constipation from my pain meds. What can we do?"
The Future of OIC Treatment
There’s new hope on the horizon. In March 2023, the FDA approved naldemedine for children as young as 12. That opens up treatment for a whole new group of patients.
And in 2024, we’ll likely see the first fixed-dose combo: naloxone + polyethylene glycol. Think of it as a pill that combines the gut-boosting power of PEG with the opioid-blocking effect of naloxone-without needing two separate medications.
By 2028, the global market for OIC treatments is expected to hit $3.4 billion. That’s because more people are living with chronic pain-and more are realizing they don’t have to suffer through constipation to manage it.
You don’t have to choose between pain control and bowel health. The tools exist. The science is clear. You just need to ask for them.
Can I just take more Miralax for opioid-induced constipation?
Miralax (polyethylene glycol) is actually one of the best first-line options for opioid-induced constipation. But taking more than 34 grams a day won’t help more-it just increases the risk of diarrhea and electrolyte imbalance. If Miralax isn’t working after 7-10 days at the full dose, it’s time to talk to your doctor about prescription options like naldemedine or naloxegol. OIC doesn’t respond the same way as regular constipation.
Is it safe to use stimulant laxatives like senna long-term for OIC?
Stimulant laxatives like senna and bisacodyl are okay for short-term use, but not ideal for long-term OIC management. They can lead to dependency, where your bowels stop responding without them. They also cause cramping and electrolyte loss. For chronic opioid users, osmotic laxatives like PEG are safer and more effective over time. Reserve stimulants for occasional rescue use only.
Why do some doctors still recommend high-fiber diets for OIC?
Many doctors follow general constipation guidelines that haven’t been updated for OIC. But opioids block gut motility, so fiber ferments instead of moving through. This causes bloating, gas, and even fecal impactions. The American Pain Society and Mayo Clinic now advise against high-fiber diets for OIC patients. If your doctor recommends it, ask for the latest guidelines-there’s strong evidence it can make your symptoms worse.
Are PAMORAs covered by insurance?
Most insurers require step therapy: you must try and fail at least two over-the-counter laxatives before they’ll approve a PAMORA like Movantik or Symcorza. Some require documentation of failed trials over 30 days. Ask your doctor’s office to help with prior authorization. Patient assistance programs from drugmakers can reduce costs to under $50/month if you qualify.
Can I take PAMORAs if I’m on methadone or buprenorphine?
Yes. PAMORAs like naldemedine and naloxegol work with all types of opioids, including methadone and buprenorphine. They don’t interfere with pain relief or addiction treatment. In fact, they’re often used in patients on opioid substitution therapy. Always check with your prescriber, but these drugs are safe and effective across the opioid spectrum.
How long does it take for PAMORAs to work?
Injectable methylnaltrexone works fastest-usually within 30 minutes to 4 hours. Oral PAMORAs like naloxegol and naldemedine take 24 to 48 hours for the first bowel movement. You won’t feel relief immediately, but most patients report consistent improvement after 3-5 days of daily use. Don’t stop too soon.
Is there a risk of withdrawal or rebound constipation with PAMORAs?
No. PAMORAs don’t cause rebound constipation or withdrawal because they don’t affect the central nervous system. They only block opioid receptors in the gut. When you stop taking them, your body returns to its baseline state-not worse. If constipation returns after stopping, it’s because the opioid is still there, not because of the PAMORA.
Managing opioid-induced constipation isn’t about enduring it. It’s about reclaiming control-over your bowels, your comfort, and your treatment. You deserve pain relief without the price of daily suffering. Ask for help. Push for answers. There are solutions that work.



 Medications
Medications



Dorine Anthony
December 21, 2025 AT 03:17I was on opioids for a year after surgery and thought I just had to deal with the constipation until I found out it wasn't normal. Started PEG daily and it was a game-changer. No more agony. Just... regular.
Also, stopped the bran cereal. Best decision ever.
Carolyn Benson
December 21, 2025 AT 23:35They say 'ask for help' like it's that simple. But what if your doctor doesn't believe you? What if they think you're just addicted and want more drugs? I've been told to 'eat more prunes' three times. I'm not lazy. I'm not weak. I'm just trapped in a system that treats pain like a moral failing.
And now they want me to pay $800 a month for a pill that 'works'? That's not medicine. That's capitalism with a stethoscope.
Aadil Munshi
December 23, 2025 AT 15:29Wow, another post telling people to take pills instead of fixing the root cause. Why not just stop opioids entirely? You're literally poisoning your gut for pain relief. It's like using a chainsaw to cut a twig.
And don't even get me started on PAMORAs - these are just fancy band-aids on a bullet wound. The real solution? Non-opioid pain management. But hey, Big Pharma loves selling you a new pill every month. 🤑
Also, Miralax isn't a cure. It's a temporary fix for a systemic failure. Wake up.
Danielle Stewart
December 23, 2025 AT 17:55If you're on long-term opioids and haven't talked to your doctor about OIC yet - please, do it today. It's not embarrassing. It's medical. You're not broken. Your body's just reacting to the medication.
Start with PEG. Track your stools. Be consistent. And if it doesn't work after two weeks, ask for naldemedine. Seriously. Your quality of life matters more than your pride.
You got this. 💪
Erica Vest
December 25, 2025 AT 06:49Clarification: The Bristol Stool Scale is a validated clinical tool, not a joke. Type 3-4 is ideal. Type 1-2 indicates severe transit delay, common in OIC. Type 5-7 suggests overuse of laxatives or PAMORA-induced diarrhea.
PEG 3350 at 17-34g/day is osmotic, not stimulant - no dependency risk. Senna is a stimulant laxative; chronic use leads to cathartic colon. Avoid unless rescue-only.
Insurance step therapy is a barrier, but documented failure of two agents (e.g., PEG + bisacodyl) is sufficient for prior authorization of Movantik or Symcorza. Ask your pharmacist to help with the paperwork.
Kinnaird Lynsey
December 27, 2025 AT 05:19Look, I get it - nobody wants to talk about poop. But if you're on opioids and you're not pooping regularly, you're not managing your pain - you're just surviving it.
And yeah, fiber sounds healthy, but for OIC? It's like throwing gasoline on a fire. I tried it. Ended up in the ER with a blockage. Never again.
PEG saved me. Naldemedine finished the job. I'm not proud of needing help. But I'm proud of getting it.
shivam seo
December 27, 2025 AT 10:08Why are we even talking about this? In Australia, we just use senna and move on. You guys make everything into a pharmaceutical industry scam. Just drink more water, eat some prunes, and stop whining.
Also, why are you paying $1,000 for a pill? You're literally paying for a patent, not a cure. Get a real life.
Andrew Kelly
December 28, 2025 AT 14:34Let me guess - you're one of those people who think the government is hiding the truth about opioids. You want us to believe these PAMORAs are safe? That they don't interfere with addiction recovery? That they're not just another way to keep people hooked on painkillers?
They're selling you a fix so you don't quit. They don't want you healed. They want you dependent on their pills. Miralax is free. Why pay for a $900 pill? You're being played.
Anna Sedervay
December 29, 2025 AT 16:49As someone who has read the full FDA label for naldemedine (yes, I did), I must say - the data is statistically significant but clinically marginal. The placebo response rate for bowel function in chronic pain cohorts is alarmingly high - up to 38% - suggesting that the perceived benefit may be confounded by regression to the mean and confirmation bias.
Also, the term "silent barrier to quality of life" is a marketing phrase, not a medical one. Please consult peer-reviewed literature, not corporate white papers.
Ashley Bliss
December 30, 2025 AT 09:50I cried the first time I had a normal bowel movement in six months after starting naldemedine. Not because I was relieved - because I realized how much I had accepted as normal.
My doctor didn't ask. My family didn't get it. I thought I was just "getting old."
But here's the truth: you don't have to suffer to be strong. You don't have to be silent to be brave.
So I'm saying it now - if you're on opioids and constipated, you deserve better. And you're not alone. I'm here. We're here.
And if you need to hear it one more time: it's not your fault. It's not weakness. It's science. And science has answers.
Moses Odumbe
December 30, 2025 AT 11:20PEG = life saver 😍
Also, stop eating kale if you're on opioids. I tried it. Felt like a balloon filled with rocks. Not worth it.
My doctor gave me Movantik - took 2 days. Now I'm back to normal. No more crying in the bathroom.
PS: Insurance made me try 3 laxatives first. F*ck step therapy. But it worked in the end. 🙏
Meenakshi Jaiswal
January 1, 2026 AT 07:05As a nurse in a pain clinic, I see this every day. Patients don't bring it up because they think it's "not a big deal." But it's the #1 reason people quit their meds.
Here's what I tell them: start PEG daily. No waiting. No "I'll take it when I feel it."
And if it doesn't work after 10 days - bring this post to your doctor. Print it. Highlight the table. Say: "I want to talk about PAMORAs."
You're not being difficult. You're being smart.