Steroid Injection Risk Calculator
Every year, intra-articular steroid injections are given to millions of people with joint pain. If you’ve been told this is a quick fix for arthritis, you’re not alone. But what if the shot that eases your knee pain today could be quietly harming your joint tomorrow? New research is flipping the script on what we thought we knew about these common treatments.
What Intra-Articular Steroid Injections Actually Do
Intra-articular steroid injections deliver powerful anti-inflammatory drugs-like triamcinolone, methylprednisolone, or betamethasone-directly into a swollen joint. The goal? Reduce pain and swelling fast. For many, relief comes within days. It’s why doctors still recommend them for osteoarthritis, especially when pain limits walking, climbing stairs, or sleeping.
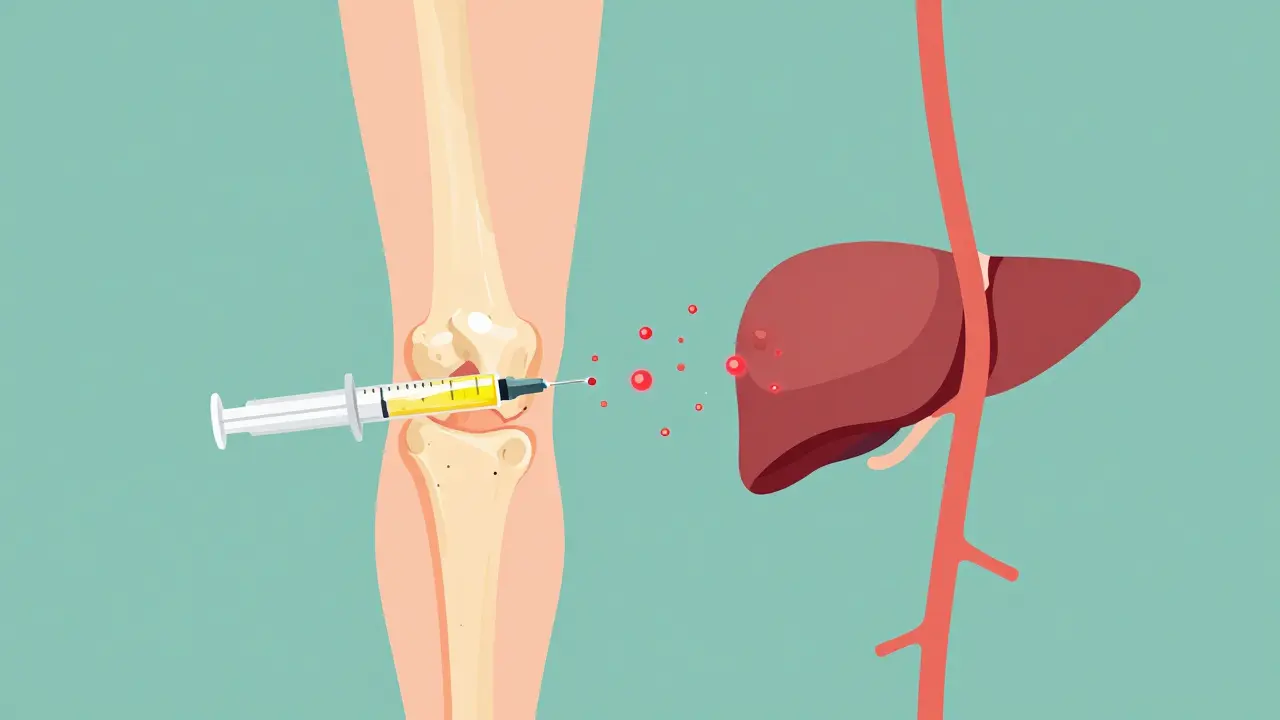
But here’s the catch: these injections aren’t just local. They don’t stay in the joint. Studies show steroids leak out into the bloodstream. That’s why you might get a facial flush, a spike in blood sugar, or even feel jittery after the shot. And while the pain relief lasts weeks, the systemic effects? They can linger for months.
The Hidden Risks: More Than Just a Temporary Flare
Most people worry about infection or a temporary flare-up after the injection. Those are real-but rare. The bigger concern isn’t what happens right after. It’s what happens over time.
A 2023 study in Radiology followed over 1,000 patients who got steroid shots in their hips or knees. The results were startling. One in 100 developed serious joint damage: bone death (osteonecrosis), stress fractures under the cartilage, or rapid joint space loss. In some cases, the joint deteriorated so fast that replacement surgery became unavoidable within just a few years.
And it’s not just one study. Data from the Osteoarthritis Initiative showed patients who got repeated steroid injections had nearly five times higher odds of visible joint damage on X-rays compared to those who didn’t. The more shots you get, the worse it gets. Three or more injections in a year? The risk climbs sharply.
Systemic Side Effects You Might Not Realize Are Connected
When steroids enter your bloodstream, they don’t just target your joint. They affect your whole body.
- High blood sugar: Even people without diabetes can see glucose levels spike after an injection. For those with type 2 diabetes, this can mean days of unstable readings and higher insulin needs.
- Bone thinning: Corticosteroids suppress bone-building cells. After multiple shots, especially in postmenopausal women, bone density can drop enough to increase fracture risk.
- Adrenal suppression: Your body makes its own cortisol. Steroid injections can trick your adrenal glands into thinking they don’t need to. This can lead to fatigue, low blood pressure, or even adrenal crisis if you get sick or have surgery soon after.
- Fluid retention and high blood pressure: Steroids cause your body to hold onto salt and water. This raises blood pressure and can worsen heart failure in vulnerable patients.
- Weight gain and Cushing-like symptoms: With frequent use, some people develop a rounded face, belly fat, or purple stretch marks-signs of excess cortisol exposure.
The Cleveland Clinic and Mayo Clinic both warn that these side effects get worse with higher doses and repeated use. And here’s something many doctors don’t mention: every injection counts. If you’re also taking oral steroids, or had a spinal injection last month, that’s part of your total steroid burden.
Who’s at Highest Risk?
Not everyone reacts the same way. Some people get a great result with no side effects. Others see damage after just one shot. Risk factors include:
- Age over 65
- Diabetes or prediabetes
- Postmenopausal women
- Obesity
- Already having moderate to severe joint damage on X-ray
- Needing surgery in the next 6-12 months
If you fall into any of these groups, you need to think harder about whether the shot is worth it. A 2023 review in PM&R says doctors should treat these patients differently-not just because of side effects, but because the injections may actually speed up joint failure in people who still have some cartilage left.

The Controversy: Why Do Doctors Still Recommend Them?
Here’s the confusing part: some studies say these injections are safe. Others say they’re dangerous. Why the contradiction?
It comes down to what you’re measuring. One study looked at pain relief. Another looked at cartilage loss on MRI. A third looked at whether people needed joint replacement. The results don’t always match.
For example, Dr. McAlindon’s 2017 study found cartilage loss after repeat shots, but no sudden bone damage. Dr. Raynauld’s trial didn’t see joint space narrowing on X-rays at all. Meanwhile, the 2023 Radiology study used advanced imaging and found clear signs of structural damage.
The American Academy of Orthopaedic Surgeons still conditionally recommends steroid injections for knee osteoarthritis. But their guideline says “conditionally”-meaning the benefits must outweigh the risks. And that’s where things get messy.
Here’s what Dr. Ali Guermazi, lead author of the key 2023 study, says: “We’ve been telling patients these injections won’t hurt your joint. But now we suspect that’s not true.”
When You Should Say No
There are times when a steroid shot is a clear win-like a sudden flare-up after a fall, or severe pain that’s blocking sleep or daily function. But here are red flags that mean you should push back:
- Your X-ray shows only mild or no arthritis-but you’re in severe pain. This might mean the pain isn’t from joint wear. Maybe it’s nerve-related, or from another condition.
- You’ve had two or more shots in the same joint in the past year.
- You’re diabetic and your blood sugar is already hard to control.
- You’re planning joint replacement surgery within the next six months.
- You’ve had a steroid shot elsewhere (like your spine or shoulder) recently.
Don’t assume the shot is harmless just because it’s “local.” The science now says it’s not.
What Are the Alternatives?
If you’re worried about steroid damage, there are other options:
- Physical therapy: Strong evidence shows it improves function and reduces pain long-term, especially for knee osteoarthritis.
- Weight loss: Losing just 5-10% of body weight can cut joint pain in half.
- Braces or orthotics: Unloader braces for the knee can shift pressure away from damaged areas.
- Viscosupplementation (hyaluronic acid): Though less effective than steroids in the short term, studies suggest it doesn’t accelerate joint damage.
- Emerging therapies: Platelet-rich plasma (PRP) and stem cell injections are being studied-but evidence is still limited and costs are high.
None of these are magic bullets. But they don’t come with the same long-term risks.

What’s the Safe Limit?
Most guidelines say: no more than 3-4 steroid injections per joint per year. But that’s a guideline, not a guarantee of safety.
The real limit? Your body’s response. If you notice your joint feels looser, more unstable, or the pain returns faster after each shot, that’s a warning sign. You’re not building tolerance-you’re wearing down the joint.
And remember: if you’ve had five shots in your knee over three years, that’s not “three a year.” That’s five. Every single one adds up.
What to Ask Your Doctor
Before you agree to a steroid shot, ask:
- “What’s the evidence this will help me long-term, not just short-term?”
- “What do my X-rays or MRI show? Is the damage mild or advanced?”
- “Could my pain be coming from somewhere else-like a tendon or nerve?”
- “What’s my total steroid exposure this year, including other shots or pills?”
- “What happens if I don’t get this shot?”
If your doctor can’t answer these clearly, get a second opinion.
The Bottom Line
Intra-articular steroid injections aren’t evil. They’ve helped millions of people walk again. But they’re not harmless, either. The idea that they’re “just a local treatment” is outdated. The data now shows they can speed up joint damage, raise blood sugar, weaken bones, and suppress your body’s natural stress response.
Use them sparingly. Use them wisely. And never assume they’re safe just because they’re common. Your joint isn’t just a place where pain lives-it’s a living structure. Treat it like one.


 Medications
Medications





Josh Potter
December 16, 2025 AT 23:56Bro, I got three of these shots last year for my knee and now I can’t even walk to the fridge without feeling like my bones are made of chalk. My sugar’s been all over the place too. Docs act like it’s a free pass, but nah. It’s a slow burn.
Radhika M
December 18, 2025 AT 16:03As a physio in Delhi, I see this all the time. People come in after their third shot, confused why their pain got worse. PT works better long-term. No side effects. Just hard work.
Jane Wei
December 19, 2025 AT 23:46My grandma got one of these and started acting like a zombie for a week. No joke. She forgot her own name. Not worth it.
CAROL MUTISO
December 21, 2025 AT 18:12Oh wow. So the medical establishment finally admitted that injecting poison into your joints might, just maybe, not be the best idea? Took them long enough. Meanwhile, my insurance still won’t cover PT. Classic.
Jigar shah
December 22, 2025 AT 22:59The data is clear: repeated steroid injections correlate with accelerated cartilage degradation, especially in patients with pre-existing structural compromise. The systemic absorption is well-documented in pharmacokinetic studies, and the suppression of endogenous cortisol production is dose- and frequency-dependent. Clinically, this necessitates a risk-benefit analysis that prioritizes long-term joint integrity over transient analgesia.
BETH VON KAUFFMANN
December 23, 2025 AT 01:59Let’s be real: if you’re getting more than one steroid injection per joint per year, you’re not managing osteoarthritis-you’re gaming the system. The AAO guidelines are vague because they’re politically neutered. Real clinicians know: if the X-ray shows joint space narrowing, you’re already past the point of no return. Stop pretending injections are ‘safe.’ They’re just delayed destruction.
Kent Peterson
December 23, 2025 AT 06:12So… you’re telling me the American healthcare system is lying to old people again? Shocking. Next you’ll say vaccines cause autism or that the moon landing was faked. I mean, come on. Steroids are fine. If your joint hurts, get the shot. If you get fat and diabetic, that’s your fault for eating pizza after the shot. Not the doctor’s. Not the drug’s. Yours.
Linda Caldwell
December 25, 2025 AT 00:07My mom got one shot last year and her hip pain vanished for 6 months. She walks without a cane now. I’m not saying it’s perfect-but it gave her back her life. Don’t throw out the baby with the bathwater.
Kaylee Esdale
December 25, 2025 AT 02:29Just because it’s a shot doesn’t mean it’s magic. I’ve seen people get 10 of these over 5 years and then wonder why they need a replacement. Your body remembers. So does your joint. Listen to your body. Move more. Lose weight. Try the brace. The shot is a Band-Aid on a broken leg.
Pawan Chaudhary
December 25, 2025 AT 12:23Bro, I’m 68 and got my first shot last month. My knee feels like new again. I’m walking to the temple again. Don’t scare people off. Sometimes you need a little help to get back on your feet. Life’s too short to sit still.
Raven C
December 26, 2025 AT 00:05How utterly pedestrian. The notion that a therapeutic intervention should be universally condemned based on aggregate population data is not only scientifically unsound-it is philosophically bankrupt. Individualized care, informed consent, and nuanced clinical judgment are the pillars of medicine-not fearmongering op-eds masquerading as peer-reviewed insight.
Erik J
December 27, 2025 AT 02:02Anyone else notice how the 2023 Radiology study used high-res MRI while the older ones used plain X-rays? That’s the real story. We’re seeing damage we couldn’t see before. Doesn’t mean the shots are evil. Just means we’re finally looking closer.