More than 1 in 4 pregnant women take herbal supplements. Not because they’re reckless, but because they’re told these are natural-and therefore safe. But herbal supplements in pregnancy aren’t regulated like prescription drugs. And that’s where the real danger lies.
What Are People Actually Taking?
Ginger tops the list. In Catalonia, nearly 3 out of 10 pregnant women use it. Why? Because it works. Multiple studies confirm that 500-1,000 mg of ginger per day reduces nausea and vomiting better than placebo, and just as well as some anti-nausea meds-without the same side effects. It’s the one herb most doctors won’t outright warn against. Then there’s raspberry leaf. You’ll find it in teas, capsules, and tinctures marketed as “uterine toners” to prep for labor. But here’s the catch: while some midwives swear by it, the American Academy of Family Physicians says it’s likely unsafe if used to induce labor. One study linked it to higher cesarean rates. And no one knows why. The dose? The timing? The plant’s growing conditions? All unknown. Chamomile is another popular choice-for sleep, for anxiety. But it’s not harmless. Evidence suggests it might interfere with fetal blood vessel development, increase preterm birth risk, or lead to low birth weight. And yet, it’s sold as a bedtime tea in grocery stores. Cranberry supplements? Used to prevent urinary tract infections (UTIs). They might help-but they’ve also been tied to spotting in the second and third trimesters. That’s not something you want to ignore. And unlike antibiotics like nitrofurantoin, which have known risks and benefits, cranberry’s safety profile is a gray zone. Rosemary? Dangerous if taken orally in medicinal amounts. It can trigger uterine contractions. But if you rub rosemary oil on your skin? No one knows if that’s safe either. The data just isn’t there.The Big Problem: No One’s Really Testing This Stuff
Pregnant women are almost never included in clinical trials. Not because researchers are cruel, but because of legal fear. If something goes wrong, lawsuits follow. So, we’re left with small studies, anecdotal reports, and centuries-old traditions passed down as fact. The U.S. FDA doesn’t require herbal supplements to prove safety or effectiveness before they hit shelves. That’s not true for prescription drugs. It’s not even true for over-the-counter painkillers like acetaminophen. But a bottle of red raspberry leaf capsules? No approval needed. No standardization. No batch testing. That means two bottles of the same brand might have wildly different amounts of active ingredients. One might contain 500 mg of raspberry leaf. The next might have 1,200 mg-or worse, unlisted contaminants like heavy metals or other herbs. A 2023 FDA inspection found that 20-60% of herbal supplements don’t contain what’s on the label. Some had no active ingredient at all. Others had toxic plants mixed in. One supplement marketed for “pregnancy support” was found to contain pennyroyal-a herb known to cause miscarriage.Why Do Women Keep Using Them?
It’s not ignorance. It’s culture. In Spain, women who used herbal supplements were 3 times more likely to believe that herbal remedies were preferable to conventional medicine. In Korea, nearly 6 in 10 pregnant women use traditional herbal formulas. In Scandinavia? Only 1 in 5. Family advice matters. A third of women in the Catalonia study started using herbs because their mothers or grandmothers told them to. Social media and Google searches were the next biggest drivers. Only 58% told their doctor. Reddit threads are full of confusion. “Is chamomile tea safe?” “I took ginger for nausea-is that okay?” “I accidentally drank rosemary tea-what do I do?” Most replies are guesses. No one has the answers.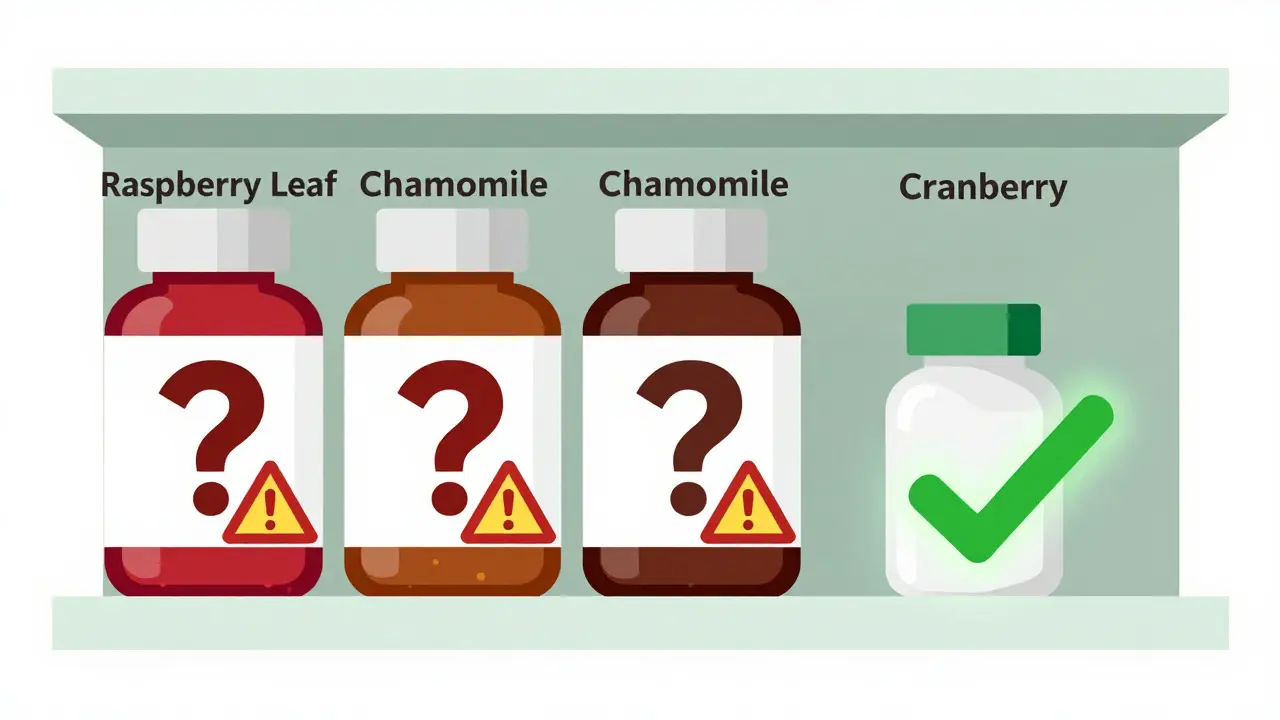
What Do Doctors Really Say?
The American College of Obstetricians and Gynecologists (ACOG) is clear: Don’t take anything without talking to your provider first. The Cleveland Clinic goes further: “People who are pregnant are encouraged to avoid most herbal supplements.” Why? Because too many have compounds that can stimulate the uterus. Too many interact with prenatal vitamins, blood thinners, or blood pressure meds. Too many have unknown effects on the developing brain or kidneys. The German Federal Institute for Risk Assessment says: “Women consuming herbal products during pregnancy are not defined by a specific profile.” That means no one type of woman uses them. It’s everywhere. And that’s why doctors need to ask-not assume. The CDC says we have “limited information to make informed treatment decisions.” That’s not a failure of the patient. It’s a failure of the system.What’s the Real Alternative?
Ginger is the exception. It’s the only herbal supplement with enough solid data to be recommended by major medical groups for nausea. Even then, they say: stick to under 1,000 mg per day. Don’t go over. Don’t mix it with blood thinners. Don’t assume more is better. For UTIs? Nitrofurantoin is still the go-to-despite its own restrictions in the third trimester. It’s tested. Its risks are known. Its benefits are clear. For anxiety or sleep? Cognitive behavioral therapy, prenatal yoga, and magnesium supplements (with doctor approval) have stronger evidence than chamomile or lavender. Prenatal vitamins? They’re regulated. They’re tested. They’re proven to reduce neural tube defects. No guesswork.
What Should You Do?
If you’re pregnant and taking herbal supplements:- Stop. Don’t panic. Just stop.
- Write down every product-name, dose, how often you take it.
- Bring that list to your next appointment. Don’t wait until you’re scared.
- Ask: “Is this safe? What’s the evidence? What happens if I stop?”
- Assume it’s unsafe until proven otherwise.
- Don’t trust marketing. Don’t trust Instagram. Don’t trust your aunt’s story.
- Check MotherToBaby.org. It’s free. It’s updated quarterly. It’s science-based.
- If your provider doesn’t know, find one who does. Not every OB-GYN is trained in herbal safety.



 Medications
Medications




Gerard Jordan
January 21, 2026 AT 20:39Just took ginger for my nausea last week 🍵😂 My grandma swears by it, but I still checked MotherToBaby.org before taking it. So glad this post exists. We need more real talk, not just Instagram moms saying 'herbs = pure magic'.
MAHENDRA MEGHWAL
January 22, 2026 AT 18:24It is indeed a matter of grave concern that herbal supplements, often consumed under the assumption of inherent safety, are not subject to the same regulatory scrutiny as pharmaceutical agents. The absence of standardized dosing and the potential for adulteration present significant risks to maternal and fetal health. A structured, evidence-based approach is imperative.
Uju Megafu
January 22, 2026 AT 20:26OMG I KNEW IT!! My cousin had a stillbirth and she was taking 'pregnancy tea' from some wellness store!! They didn't even test it!! This is why I don't trust 'natural' anything!! WOMEN ARE DYING BECAUSE THEY TRUST AMAZON REVIEWS!!
Barbara Mahone
January 24, 2026 AT 01:32Chamomile tea in moderation-brewed from loose leaves, not supplements-is likely low-risk. The real danger lies in concentrated extracts and unregulated capsules. The distinction matters.
Kelly McRainey Moore
January 25, 2026 AT 20:36I used ginger and chamomile during both pregnancies. Felt fine. But I also talked to my midwife every time I added something new. Not everyone has that access, which is why this info matters so much.
Amber Lane
January 26, 2026 AT 01:00Ginger works. Everything else? Play it safe. Stop. Ask. Wait.
Ashok Sakra
January 27, 2026 AT 05:11Why they not ban all herbs? Why let people poison babies? I heard one woman took rosemary and her baby came out with no nose. Is that true? I need to know!
Andrew Rinaldi
January 27, 2026 AT 11:53We’re stuck between tradition and science. Neither side has all the answers. But the system that lets untested products flood the market while pregnant people are left guessing? That’s the real failure.
michelle Brownsea
January 28, 2026 AT 06:59Let me be perfectly clear: if you’re pregnant and you’re taking anything that isn’t FDA-approved, you’re gambling with your child’s life. And no, 'natural' doesn’t mean 'safe.' It means 'unregulated.' And if your doctor doesn’t scare you enough about this, find a new one. This isn’t a lifestyle choice-it’s negligence dressed up as wellness.
Roisin Kelly
January 28, 2026 AT 23:27They're lying. The FDA knows exactly what's in these supplements. They just don't care because Big Herbal is paying them. I read a leak last year-there's a whole backdoor list of banned herbs they won't touch because they're 'too profitable.' You think your chamomile tea is innocent? It's not. They're letting us die so they can sell more.