When your stomach hurts after eating, and you feel bloated, nauseous, or like you’re burning from the inside, it’s easy to blame spicy food or stress. But if those symptoms stick around, it might be something deeper: gastritis. This isn’t just an upset stomach-it’s inflammation of the stomach lining, a protective barrier that normally shields your stomach from its own powerful digestive acids. When that lining gets damaged, pain, bleeding, and even long-term complications can follow. And in most cases, the culprit is a tiny bacterium most people have never heard of: Helicobacter pylori.
What Exactly Is Gastritis?
Gastritis means your stomach lining is inflamed. Think of it like a sunburn, but inside your stomach. The lining, called the mucosa, is supposed to be tough enough to handle stomach acid. But when it gets irritated or infected, it swells up, becomes sensitive, and can even break down. That’s when you start feeling pain, nausea, or a burning sensation right below your ribs. There are two main types: erosive and nonerosive. Erosive gastritis means there are actual breaks or sores in the lining-these can bleed, which is why some people notice black, tarry stools or even vomit blood. Nonerosive gastritis doesn’t show visible damage, but the cells underneath are still changing. This type often happens slowly, over years, and many people don’t even know they have it until they get tested. About 70 to 90% of all gastric ulcers and most cases of chronic gastritis are tied to H. pylori. This bacteria lives in the stomach, survives the acid, and sticks to the lining like glue. Over time, it triggers an immune response that turns into long-term inflammation. In fact, if you have H. pylori, your risk of developing stomach cancer goes up by 6 to 8 times. That’s why treating it isn’t just about feeling better-it’s about preventing serious disease.How Do You Know If You Have H. pylori?
Most people with H. pylori don’t have symptoms at first. It can hang around for years without causing trouble. But when it does, signs include:- Upper abdominal pain or burning, especially when hungry or at night
- Nausea or vomiting
- Bloating or feeling full after eating just a little
- Loss of appetite
- Unexplained weight loss
How Is H. pylori Treated?
Treating H. pylori isn’t as simple as popping an antibiotic. This bug is stubborn. It’s surrounded by a protective layer and lives in a super acidic environment. So, doctors use a combo approach called triple therapy: one proton pump inhibitor (PPI) to shut down acid production, plus two antibiotics to kill the bacteria. Common antibiotics used are amoxicillin and clarithromycin. The treatment lasts 10 to 14 days. If it works, the bacteria are wiped out, the stomach lining heals, and symptoms usually improve within days. Success rates? Around 80 to 90% in places where antibiotics still work well. But here’s the problem: antibiotic resistance is rising. In the U.S., clarithromycin resistance has jumped from 10% in 2000 to 35% today. That means one in three people might get a treatment that doesn’t work. In places like Australia, where resistance is moderate, doctors now often use bismuth quadruple therapy instead: a PPI, bismuth, metronidazole, and tetracycline. This combo hits the bacteria from multiple angles and works better where clarithromycin fails. In 2022, the FDA approved a new drug called vonoprazan (brand name Voquezna). It’s not an antibiotic-it’s a potassium-competitive acid blocker, which stops acid even better than PPIs. In clinical trials, vonoprazan-based therapy cleared H. pylori in over 90% of cases, even after two failed treatments. It’s becoming a go-to option for stubborn infections.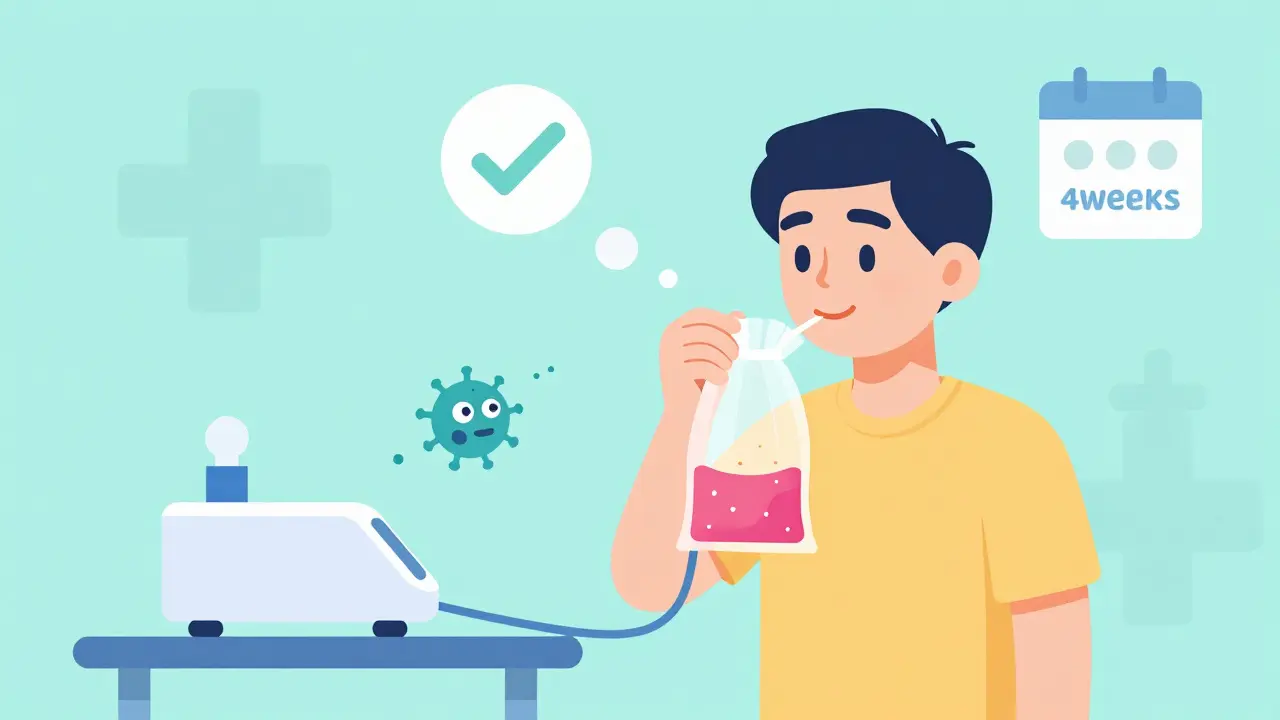
What About Other Causes of Gastritis?
Not all gastritis comes from H. pylori. About 25 to 30% of cases are caused by NSAIDs-common painkillers like ibuprofen, naproxen, or even daily aspirin. These drugs block protective chemicals in the stomach lining, leaving it exposed to acid. If you’re on these regularly for arthritis or heart health, talk to your doctor about switching to safer options or adding a PPI for protection. Alcohol is another big one. Drinking more than 30 grams a day (about two standard drinks) doubles your risk. Quitting alcohol can reduce symptoms by 60% in just two weeks. Then there’s autoimmune gastritis. This rare form happens when your immune system attacks your own stomach cells, especially the ones that make acid and intrinsic factor (needed for vitamin B12 absorption). It’s often linked to other autoimmune diseases like Hashimoto’s thyroiditis. People with this type need lifelong B12 shots or supplements because their body can’t absorb it from food anymore.What Happens After Treatment?
You finish your antibiotics, feel better, and think you’re done. But you’re not. You need to confirm the bacteria is gone. That’s why doctors recommend a urea breath test 4 weeks after finishing treatment. Testing too soon can give false negatives because the bacteria might be dormant, not dead. If treatment fails, your doctor will try a different combo-usually switching antibiotics based on local resistance patterns. Some patients need a third round, or even endoscopic monitoring if they have a family history of stomach cancer. Another issue: rebound acid. If you’ve been on PPIs for months or years, stopping suddenly can cause your stomach to overproduce acid. That’s not because the infection came back-it’s because your body got used to less acid and went into overdrive. This can feel like your gastritis is flaring up again. The fix? Taper off slowly under medical supervision, not cold turkey.Lifestyle Changes That Actually Help
Medication works best when paired with smart habits:- Stop NSAIDs if possible-use acetaminophen instead for pain.
- Avoid alcohol entirely during treatment and ideally long-term.
- Quit smoking-it slows healing and increases cancer risk.
- Eat smaller meals-large meals stretch the stomach and worsen discomfort.
- Avoid spicy, acidic, or fried foods if they trigger symptoms. They don’t cause gastritis, but they irritate the lining.

When Should You Worry?
Most gastritis isn’t an emergency. But some signs mean you need help right away:- Black, tarry stools (melena)-a sign of internal bleeding
- Vomiting blood or material that looks like coffee grounds
- Sudden, severe abdominal pain
- Dizziness, rapid heartbeat, or extreme fatigue-signs of anemia from chronic blood loss
Why This Matters Now
H. pylori infection is declining in younger generations thanks to better hygiene and antibiotics, but it’s still common in older adults and in parts of the world with limited healthcare access. In Australia, about 20% of people over 60 carry it. The good news? Treating it cuts your risk of stomach cancer by half. The challenge? Many people still get diagnosed too late. On average, people wait over 8 months before seeing a doctor for persistent symptoms. And too many end up with unnecessary endoscopies because doctors don’t test for H. pylori first. The smartest move? If you’re over 40 and have recurring stomach issues, ask for a breath test. It’s quick, non-invasive, and could save your life.What’s Next for Gastritis Treatment?
Researchers are working on personalized treatments. Instead of giving everyone the same antibiotics, they’re testing the bacteria’s genetic makeup to pick the most effective drugs. Early trials show success rates hitting 95% when treatment is tailored to the strain. New drugs are coming too. Beyond vonoprazan, scientists are exploring bacteriophages (viruses that target bacteria) and probiotics that can help restore the gut after antibiotics. The goal isn’t just to kill H. pylori-it’s to rebuild a healthy stomach environment so it doesn’t come back. For now, the best strategy is simple: test early, treat correctly, follow up, and protect your stomach. It’s not just about comfort-it’s about long-term health.Can gastritis go away on its own?
Sometimes, especially if it’s caused by a short-term trigger like alcohol or NSAIDs, mild gastritis can improve if you remove the irritant. But if it’s caused by H. pylori, it won’t go away on its own. Left untreated, it can lead to ulcers, bleeding, or even stomach cancer. Testing and treatment are essential for long-term healing.
Is H. pylori contagious?
Yes. H. pylori spreads through contaminated food, water, or close contact like kissing or sharing utensils. It’s more common in areas with poor sanitation. Many people get infected in childhood. Once you have it, you’re unlikely to catch it again after successful treatment.
Can I drink alcohol with gastritis?
No-not during treatment, and ideally not long-term. Alcohol irritates the stomach lining and can make inflammation worse. Even moderate drinking can delay healing and increase the risk of bleeding. If you have gastritis, avoid alcohol until your doctor says it’s safe.
Do I need to take PPIs forever?
No. PPIs are used short-term to help your stomach heal during treatment. Long-term use (over a year) can cause side effects like nutrient deficiencies, bone loss, or rebound acid. Only continue if you have a confirmed medical need, like recurring ulcers or severe reflux. Always taper off under your doctor’s guidance.
How do I know if my H. pylori treatment worked?
You need a follow-up test-usually a urea breath test-4 weeks after finishing antibiotics. Symptoms alone aren’t reliable. Even if you feel better, the bacteria might still be there. Confirming eradication prevents future complications and avoids unnecessary repeat treatments.
Can stress cause gastritis?
Stress doesn’t directly cause H. pylori gastritis, but it can worsen symptoms and slow healing. Severe physical stress-like from major surgery, burns, or critical illness-can cause acute erosive gastritis. Emotional stress alone is unlikely to be the main cause, but managing it helps overall recovery.



 Medications
Medications





Bobby Collins
January 2, 2026 AT 02:39Okay but have you ever wondered if H. pylori is just a cover-up for glyphosate poisoning? The government and Big Pharma don’t want you to know that Roundup alters your gut flora and makes you susceptible to ‘bacteria’-it’s all engineered. They profit off antibiotics and endoscopies. The breath test? Probably calibrated to confirm their narrative. 🤔
Donna Peplinskie
January 3, 2026 AT 11:48I just want to say-thank you for writing this so clearly. I’ve been dealing with bloating for years, and no one ever explained it like this. I finally got tested last month, and it was H. pylori. Triple therapy worked, but I cried when I realized how long I waited to get help. You’re not alone. Please, if you’re reading this and feel ‘just tired’ or ‘a little off’ after meals-get tested. It’s not ‘just stress.’
Liam George
January 4, 2026 AT 05:15Let’s deconstruct the paradigm: H. pylori isn’t a pathogen-it’s a symbiont that’s been pathologized by the medical-industrial complex. The stomach’s acidity evolved to regulate microbial colonization, not eradicate it. When you suppress acid with PPIs, you disrupt the entire enteric ecosystem. Vonoprazan? Just a more elegant tool for systemic dysbiosis. The real cure is ancestral diet restoration and vagal toning. The data is there-if you know where to look.
sharad vyas
January 5, 2026 AT 01:17In India, we used to treat stomach pain with ginger tea and fasting. My grandfather said, 'The body knows how to heal if you let it rest.' Now we swallow pills like candy. Maybe we lost something important. Not saying antibiotics are bad-but maybe we should listen to older ways too.
Dusty Weeks
January 6, 2026 AT 18:44so i tried the breath test and it was neg but i still feel like crap… maybe its the 5g? or the new airpods? i think my stomach is being hacked… 🤯
Sally Denham-Vaughan
January 6, 2026 AT 21:41OMG I’m so glad this post exists. I was just telling my sister yesterday how I thought I was ‘just a nervous eater’ until I got diagnosed with H. pylori. I didn’t even know it could be passed through kissing. Now I’m telling everyone. Seriously-get tested if you’ve had stomach issues for more than a few weeks. It’s not dramatic, it’s just… common. And treatable.
Bill Medley
January 8, 2026 AT 16:02Testing for H. pylori prior to endoscopy is standard of care. Failure to do so constitutes a deviation from clinical guidelines.
Richard Thomas
January 9, 2026 AT 00:26It’s fascinating how we’ve reduced a complex biological interaction to a binary ‘bug = bad’ narrative. H. pylori has coexisted with humans for tens of thousands of years. Its decline in modern populations correlates with rising rates of esophageal adenocarcinoma, asthma, and allergies. Perhaps it’s not the villain, but the ghost of a balanced microbiome we’ve lost. Treatment is necessary when symptomatic-but should we be so quick to eradicate what once kept us whole?
Paul Ong
January 10, 2026 AT 19:06Quit the NSAIDs. Stop the booze. Eat smaller meals. That’s it. No magic. No conspiracy. Just basic respect for your body. Done. 🙌
Andy Heinlein
January 11, 2026 AT 00:40i got treated last year and i feel like a new person!! no more bloating after lunch, no more midnight stomach burns. i used to think i was just ‘sensitive’ but turns out i had a tiny invisible enemy inside me. you guys should get tested!! it’s easy and life changing!! 🎉❤️
Ann Romine
January 12, 2026 AT 07:32I’m from the Philippines. In my village, everyone drinks boiled water and eats fermented foods. No one here gets H. pylori. But when my cousin moved to the city and started eating fast food and bottled drinks, she got sick. Maybe it’s not just the bacteria-it’s the whole way we live now.
Austin Mac-Anabraba
January 13, 2026 AT 06:30Let’s be honest: 90% of people who get diagnosed with H. pylori are middle-aged, overweight, and on PPIs. They’re the ones who ignore lifestyle factors and then expect a pill to fix everything. You don’t need a breath test-you need a new diet, a walk after dinner, and to stop using ibuprofen like candy. This post reads like a pharmaceutical brochure.