Black Box Warning Checker
Enter any prescription drug name to check if it has the FDA's strongest safety alert. This tool helps you understand what a black box warning means for your medication.
How Black Box Warnings Work
The FDA issues black box warnings for drugs with serious risks. These aren't warnings to avoid the drug completely, but rather signals that you and your doctor should carefully consider the benefits versus risks.
When you pick up a prescription, you probably don’t think about the tiny black rectangle on the drug label. But that box? It’s the FDA’s loudest alarm bell. A black box warning is the strongest safety alert the U.S. Food and Drug Administration can issue. It doesn’t mean the drug is unsafe for everyone. It means the risks are serious enough that doctors must pause, think, and talk to you before prescribing it.
What Exactly Is a Black Box Warning?
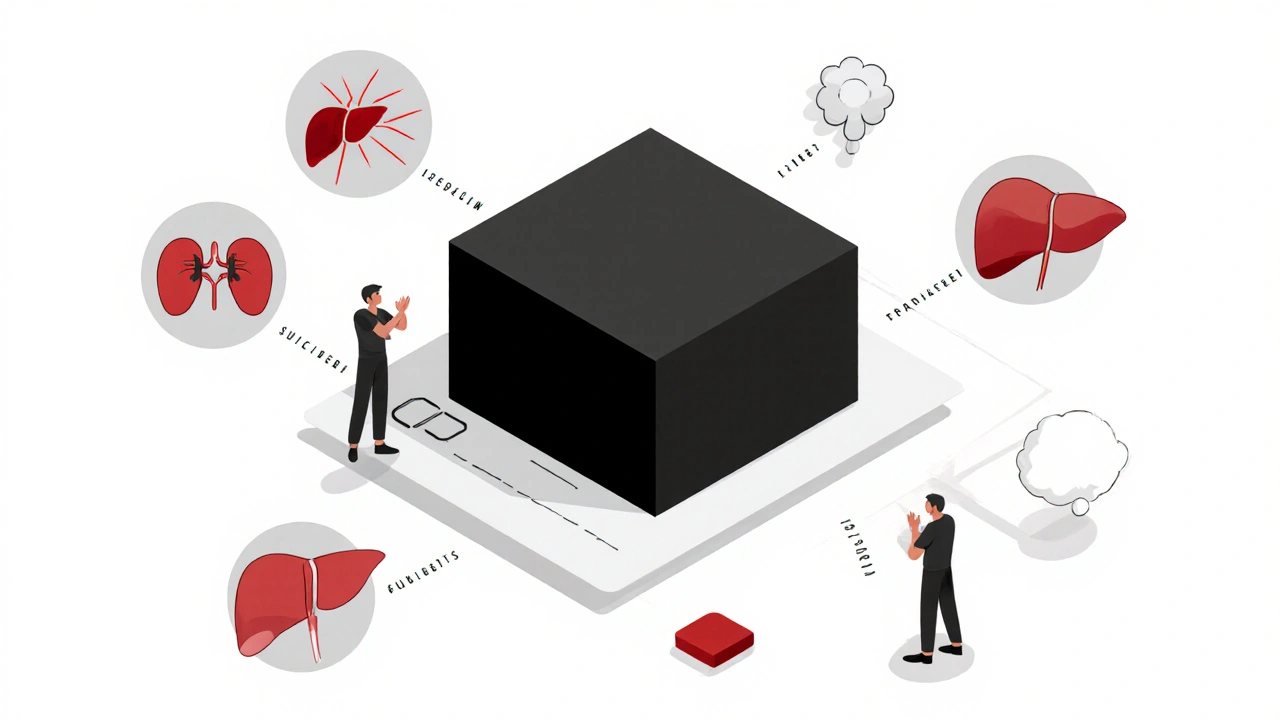
A black box warning is a highlighted section in a drug’s official prescribing information. It’s printed in a thick black border-like a warning sign on a construction site-and appears right after the drug’s introduction. This isn’t just a footnote. It’s the FDA’s way of saying: “This drug can kill or cause life-altering harm.” These warnings aren’t random. They’re based on real evidence-data from clinical trials, post-market reports, and long-term studies. The FDA only puts a black box on a drug when the risk is clear, severe, and preventable. Think: sudden heart failure, suicidal thoughts, liver damage, or severe allergic reactions that lead to death. As of 2022, more than 400 prescription drugs carried a black box warning. That includes medications for depression, diabetes, arthritis, epilepsy, and even some antibiotics. The warning doesn’t mean the drug is banned. It means the benefits must clearly outweigh the risks-and only a trained professional should decide that.Why Do These Warnings Exist?
The black box system started in the 1960s after a series of drug disasters. The Kefauver-Harris Amendments of 1962 gave the FDA power to demand proof of safety before a drug could be sold. But it wasn’t until later that the black box format became standard. The goal? To stop preventable deaths. For example, the diabetes drug rosiglitazone (Avandia) got a black box warning in 2007 after studies linked it to heart attacks. After the warning, prescriptions dropped by 70%. But here’s the twist: another similar drug, pioglitazone, got the same warning a year later-and prescriptions barely changed. Why? Media coverage. Public panic. Doctors’ habits. The warning alone isn’t enough. It needs context. Black box warnings are meant to force a conversation. Not to scare you off a drug, but to make sure you and your doctor understand the stakes. Some warnings say: “Don’t use if you have liver disease.” Others say: “Monitor blood counts every two weeks.” A few say: “Avoid in patients under 24 due to increased suicide risk.”How the FDA Decides to Issue a Warning
The FDA doesn’t slap on a black box warning lightly. It’s a multi-step process:- Lab and animal testing shows early red flags.
- Clinical trials in humans reveal side effects-but sometimes only in small groups.
- Post-market monitoring is where most black box warnings come from. Once a drug is used by millions, rare but deadly reactions show up.
- FAERS data (the FDA Adverse Event Reporting System) collects reports from doctors, patients, and pharmacies. If enough people report the same serious side effect, the FDA investigates.
- Expert review decides if the risk is serious enough to warrant a black box. If yes, the drugmaker must update the label.
What’s in a Black Box Warning?
Not all black box warnings are the same. They usually include:- Specific risks-like “risk of suicidal behavior in children and adolescents” (common with antidepressants).
- Contraindications-who should NOT take the drug. For example, “avoid in patients with a history of heart failure.”
- Monitoring requirements-“Check liver enzymes monthly,” or “Measure blood pressure before each dose.”
- Special population restrictions-“Not recommended for pregnant women,” or “Use only in adults over 65 under close supervision.”
How Doctors Use These Warnings
Doctors don’t ignore black box warnings. They use them as a checklist. The American Academy of Family Physicians recommends the STEPS approach when considering a drug with a black box:- Safety: What are the risks?
- Tolerability: Can the patient handle side effects?
- Effectiveness: Does it work better than alternatives?
- Price: Is there a cheaper, safer option?
- Simplicity: How hard is it to take correctly?
What You Should Do If Your Drug Has a Black Box Warning
If your prescription has a black box warning, don’t panic. But do ask questions:- What’s the specific risk? Is it heart failure? Liver damage? Suicidal thoughts?
- How likely is it? Is it 1 in 100? 1 in 1,000? The warning doesn’t tell you the odds-ask for numbers.
- What monitoring do I need? Blood tests? Appointments? Scans?
- Are there safer alternatives? Even if they’re less effective, are they better for your situation?
- What happens if I stop? Could my condition get worse without this drug?
What About Over-the-Counter Drugs?
Black box warnings only apply to prescription drugs. You won’t see them on aspirin, allergy pills, or sleep aids. That’s because the FDA regulates OTC medications differently-they’re assumed to be safe for self-use with clear labeling. But that doesn’t mean OTC drugs are risk-free. Some can still cause serious harm if misused. For example, taking too much acetaminophen (Tylenol) can cause liver failure. That’s why the label says “Do not exceed 4,000 mg per day.” The difference? A black box warning is a federal mandate. An OTC warning is just a label. The FDA doesn’t require black boxes for non-prescription drugs because they’re meant for short-term, low-risk use.
How the System Is Changing
The FDA knows black box warnings aren’t perfect. Studies show they don’t always change behavior. Some doctors skip reading them. Some patients ignore them. Others panic and stop taking life-saving meds. So the agency is working on improvements:- More plain language-less jargon.
- Clearer risk numbers-not just “serious risk,” but “1 in 500 chance.”
- Better digital labeling so warnings pop up in electronic prescriptions.
- More patient-friendly summaries to hand out at pharmacies.
Where to Find Updated Warning Info
Drug labels change. A warning you saw last year might be updated today. Here’s where to check:- Drugs@FDA - The FDA’s official database of drug labels.
- Drug Effectiveness Review Project - Independent analysis of drug safety and effectiveness.
- Consumer Reports Best Buy Drugs - Compares drugs by cost, safety, and results.
- MedWatch - Report side effects yourself. Your report could help trigger a new warning.
Final Thought: It’s About Awareness, Not Fear
A black box warning isn’t a death sentence. It’s a signal. A red flag. A reason to talk, not to run. Some of the most effective drugs in medicine carry black box warnings. They save lives-but only if used correctly. If your doctor prescribes a drug with a black box, don’t assume they’re cutting corners. They’re likely weighing the best option for you-even if it’s risky. Your job? Ask questions. Track side effects. Report anything unusual. And never stop the drug without talking to your provider. Because in medicine, the strongest warning isn’t the one in the box. It’s the one you ignore.What does a black box warning mean for my health?
A black box warning means the drug carries a serious risk of death or severe injury. It doesn’t mean you can’t take it-but you and your doctor must carefully weigh the benefits against the risks. The warning exists to make sure you’re fully informed before starting the medication.
Do all prescription drugs have black box warnings?
No. Only about 1 in 10 prescription drugs in the U.S. carry a black box warning. These are reserved for medications with the most serious, well-documented risks-like heart failure, liver damage, or suicidal behavior. Most common drugs like blood pressure or antibiotic pills don’t need one.
Can I still take a drug with a black box warning if I need it?
Yes, if your doctor believes the benefits outweigh the risks. Many life-saving drugs-like clozapine for schizophrenia or certain chemotherapy agents-have black box warnings. The key is monitoring: regular blood tests, doctor visits, and reporting side effects early. Never stop taking it without talking to your provider.
How do I know if my drug has a black box warning?
Check the printed patient information sheet that comes with your prescription. It’s always near the top, in a black-bordered box. You can also search the drug name on [email protected] or ask your pharmacist. If you’re using an online pharmacy, the warning should appear in the product description.
Can I report a side effect from a drug with a black box warning?
Yes, and you should. The FDA uses the MedWatch program to collect reports from patients and doctors. If enough people report the same serious side effect, it could lead to a stronger warning or even a drug recall. You can report online at fda.gov/medwatch or call 1-800-FDA-1088.
Are black box warnings the same worldwide?
No. The U.S. FDA uses the black box format, but other countries have different systems. The European Medicines Agency uses “contraindications” and “warnings” without the black border. Canada and Australia use similar risk categories but don’t have an exact equivalent. Always check local guidelines if you’re traveling or using imported medications.


 Medications
Medications


Destiny Annamaria
November 19, 2025 AT 10:26My grandma’s on a black box drug for her arthritis and she swears by it-says it’s the only thing that lets her garden again. She gets her blood checked every month like clockwork. I used to freak out every time she mentioned it, but now I get it. It’s not about fear, it’s about awareness. She’s alive and kicking because she didn’t ignore the box.
Bharat Alasandi
November 20, 2025 AT 17:25Bro, black box = FDA’s way of saying ‘this shit can kill u if u dumb’ but also ‘u might need it anyway.’ Like clozapine? It’s basically a nuclear option for schizophrenia-but if ur brain’s on fire and everything else failed, you take it. Monitoring = your new best friend. Check labs. Report weird dreams. Don’t be that guy who ghosts his psych appointment.
Kristi Bennardo
November 21, 2025 AT 00:45This entire system is a catastrophic failure of pharmaceutical oversight. The FDA waits until people are DEAD before they act. And then they slap on a black box like it’s a sticker on a cereal box. Where was this warning when my cousin died from that antidepressant? The system is broken. Corporate greed. Regulatory capture. Wake up, people.
Shiv Karan Singh
November 21, 2025 AT 06:40LMAO black box warnings. 😂 Like anyone reads them. My cousin took that diabetes med with the warning and still drank 6 beers a night. He’s fine. Probably just scared the FDA into making more paperwork. Real danger? The 1000 other drugs they don’t warn you about. 🤷♂️
Ravi boy
November 23, 2025 AT 04:38black box = dont panic but dont ignore either. my uncle took the epilepsy med with the warning and it saved his life. he checks his liver every 2 weeks. its not scary its just info. doctors are not trying to kill you. theyre trying to help. dont be scared of the box be scared of not asking questions
daniel lopez
November 23, 2025 AT 21:11EVERY black box warning is a cover-up. The FDA and Big Pharma know these drugs are poison but they keep them on the market because they make billions. The ‘monitoring’? A joke. You think your doctor’s actually checking your blood? Nah. They’re paid by the pharma reps. You’re a lab rat. Wake up. The truth is hidden in plain sight.
Nosipho Mbambo
November 24, 2025 AT 02:35...I just read this whole thing... and honestly... I don’t know... I mean... I guess... it’s something...? I’m just here for the memes. Why is this so long? I didn’t ask for a textbook. 🤷♀️
Katie Magnus
November 25, 2025 AT 21:33So let me get this straight. You’re telling me the government says a drug might kill me… but I can still take it? How is that not a violation of basic human rights? I mean, if it’s that dangerous, why isn’t it banned? This is just corporate propaganda dressed up as medicine.
King Over
November 26, 2025 AT 05:43My doc gave me a black box med for my anxiety. I asked what the risk was. He said 1 in 500. I said okay. I take it. I sleep. I function. The box is just a reminder to stay alert. Not a reason to quit. Simple.
Johannah Lavin
November 26, 2025 AT 16:44Just wanted to say-thank you for writing this. 🙏 My mom was terrified when her doctor prescribed her a black box drug for her autoimmune condition. I showed her this and she cried. Not from fear-from relief. She finally understood it wasn’t a death sentence, it was a roadmap. You made people feel seen. 💙
Ravinder Singh
November 28, 2025 AT 07:46Love how this breaks it down. Seriously. Black box ain’t a stop sign-it’s a detour sign. Like, yeah, there’s a landslide ahead, but the other road’s blocked too. So you drive slow, check the mirrors, call your mechanic. Same with meds. You don’t ditch the ride-you just upgrade your driving habits. 🚗💨
Russ Bergeman
November 28, 2025 AT 10:31Wait, so you’re saying the FDA doesn’t test drugs properly before they’re sold? And then, after people die, they slap on a warning? That’s not safety. That’s negligence. And your doctor? They’re just following the script. You’re not a patient-you’re a revenue stream. I’m not taking anything with a black box. Ever.