When your heart skips, races, or feels like it’s fluttering in your chest, it’s not just uncomfortable-it can be dangerous. Atrial fibrillation (AFib) is the most common type of irregular heartbeat, affecting millions worldwide. And while many people think of it as just a nuisance, the real danger lies in one thing: stroke. People with AFib are five times more likely to have a stroke than those with a normal heartbeat. That’s why how you treat it matters just as much as diagnosing it.
Two Ways to Tackle AFib: Rate or Rhythm?
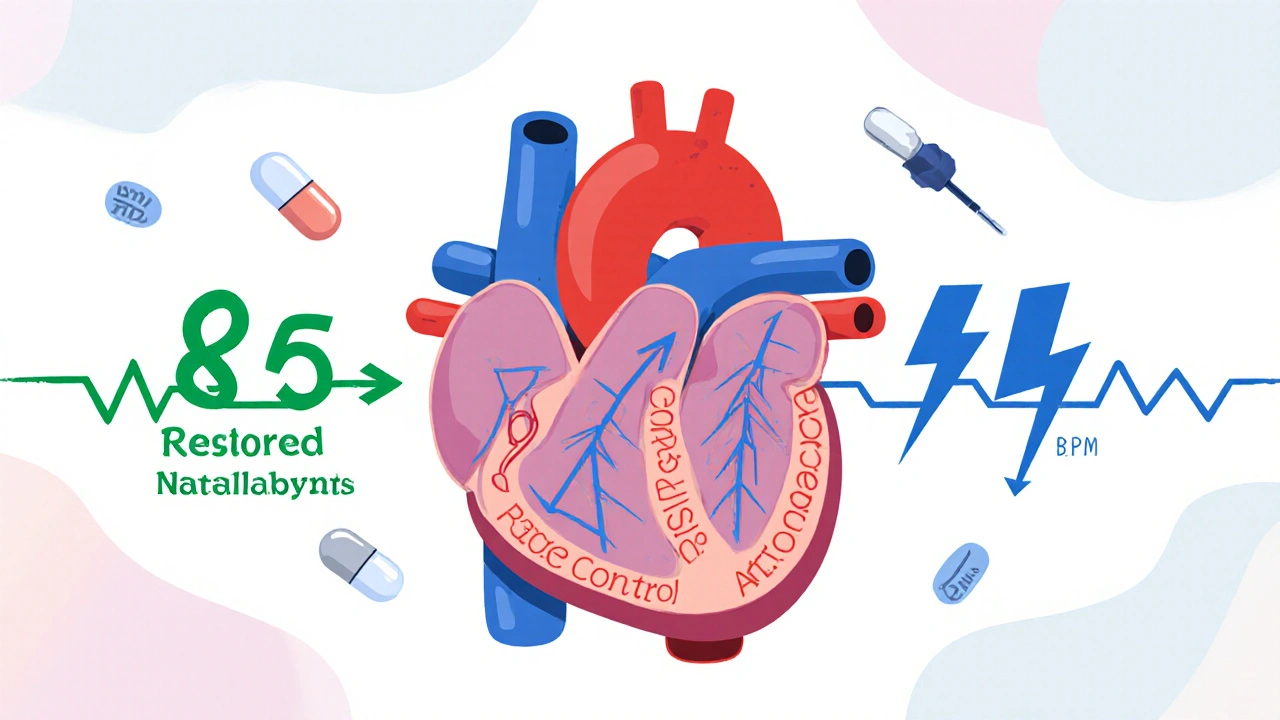
There are two main strategies doctors use to manage AFib: rate control and rhythm control. They’re not competing goals-they’re tools. And which one you need depends on your age, symptoms, heart health, and even how long you’ve had AFib.Rate control doesn’t try to fix your heartbeat. Instead, it slows it down to a safer pace. Your heart might still be irregular, but if it’s not racing at 150 beats per minute, your body can cope better. The goal? Keep your resting heart rate below 110 beats per minute. Surprisingly, studies like the RACE II trial found that being a little looser with the target-letting it go up to 110-is just as safe as trying to keep it under 80. That’s good news because it means fewer pills, fewer side effects, and less stress over perfect numbers.
Medications for rate control are simple: beta-blockers like metoprolol, calcium channel blockers like diltiazem, or digoxin. These are old-school drugs, well-tested, and generally safe. They’re often the first choice, especially for older adults or those with other health problems like kidney disease or COPD.
On the other side is rhythm control. This strategy tries to get your heart back into its normal rhythm-sinus rhythm-and keep it there. That means using drugs like amiodarone, flecainide, or dronedarone. Or, more commonly now, going straight to a procedure: electrical cardioversion (a quick electric shock to reset your heart) or catheter ablation (a tiny wire burned into the heart to block the faulty signals).
Why Did Doctors Used to Prefer Rate Control?
Back in the early 2000s, the AFFIRM trial changed everything. It followed over 4,000 patients with AFib for years and found no difference in death rates between those on rate control and those on rhythm control. In fact, the rhythm control group had more hospital visits and more side effects from antiarrhythmic drugs. So for a long time, doctors told patients: don’t bother trying to fix the rhythm. Just slow the heart down and take blood thinners to prevent stroke.That advice stuck for nearly two decades. But here’s the problem: those early trials didn’t have the tools we have today. The drugs were harsher. Ablation procedures had complication rates as high as 20%. And most patients in those studies were older-with lots of other health issues.
The Big Shift: Why Rhythm Control Is Coming Back
In 2020, everything changed with the EAST-AFNET 4 trial. This study looked at 2,785 people who had been diagnosed with AFib within the past year. Half got rhythm control early-within 12 months of diagnosis. The other half got the old-school rate control approach.The results? A 21% lower risk of death, stroke, heart failure hospitalizations, or heart attacks in the early rhythm control group. That’s not a small difference. It’s life-changing. And it wasn’t just for people with symptoms. Even those who felt fine benefited.
That’s why the European Society of Cardiology updated its guidelines in 2023. They now say: if you’ve just been diagnosed with AFib, consider rhythm control-not just if you’re struggling with symptoms, but as a first option. Especially if you’re under 75, have heart failure, or are at higher risk for stroke.

Who Should Get Rhythm Control?
Not everyone needs to chase a normal rhythm. But if you fit any of these profiles, rhythm control deserves serious consideration:- You’re under 65
- Your AFib started recently (within the last year)
- You have symptoms like fatigue, dizziness, or shortness of breath
- You have heart failure, even if it’s mild
- Your CHA₂DS₂-VASc score is 2 or higher (that’s a tool doctors use to measure stroke risk)
For these people, rhythm control isn’t just about feeling better-it’s about living longer. Ablation success rates today are over 80% for paroxysmal AFib (the kind that comes and goes), and complication rates have dropped below 5%. That’s a huge leap from 20 years ago.
Who Should Stick With Rate Control?
Rate control isn’t outdated. It’s still the right choice for many:- You’re over 75
- You have multiple health problems like kidney disease, lung disease, or diabetes
- Your AFib is permanent and you don’t feel symptoms
- You’re not a good candidate for ablation (due to anatomy, previous surgery, or other risks)
For these patients, the risks of antiarrhythmic drugs or invasive procedures often outweigh the benefits. Slowing the heart down with a simple pill and staying on blood thinners is safer, simpler, and just as effective at preventing death.

Stroke Prevention: The One Thing That Never Changes
No matter which strategy you choose-rate or rhythm-you still need blood thinners. This is non-negotiable. AFib doesn’t care if your heart is in rhythm or not. If the top chambers aren’t beating properly, blood pools and clots form. And clots mean strokes.Doctors use the CHA₂DS₂-VASc score to decide who needs anticoagulants. A score of 2 or higher? You need a blood thinner. That’s true even if you’re in sinus rhythm after an ablation. Studies show that many strokes happen because people stopped their blood thinners too soon.
Common blood thinners today include apixaban, rivaroxaban, and dabigatran. They’re easier to manage than warfarin, don’t need constant blood tests, and have fewer food interactions. But they’re not risk-free. Bleeding is still a concern, especially in older adults. That’s why your doctor will check your kidney function, fall risk, and history of bleeding before starting you on one.
What About the Future?
The next big thing isn’t just more ablations-it’s smarter ablations. New mapping technologies let doctors see exactly where the faulty signals are coming from. There’s even research into using AI to predict which patients will respond best to ablation before the procedure even starts.Trials like ASSERT II are now looking at whether early rhythm control helps people with heart failure and preserved ejection fraction-a group that didn’t benefit much in past studies. Results are expected in 2025.
And the market is catching up. The global ablation device market is growing fast-projected to hit $6.2 billion by 2028. That means more access, better tech, and lower costs over time.
What Should You Do?
If you’ve been diagnosed with AFib, don’t panic. But don’t accept the first answer you hear, either. Ask your doctor:- What’s my CHA₂DS₂-VASc score?
- How long have I had AFib?
- Am I a candidate for ablation?
- What are the risks and benefits of rhythm control for someone like me?
- Can we try rhythm control early-even if I don’t feel symptoms?
There’s no one-size-fits-all plan. But the days of automatically choosing rate control are over. If you’re young, otherwise healthy, and diagnosed early, rhythm control might be the best way to protect your heart-and your future.


 Medications
Medications




Melania Rubio Moreno
November 26, 2025 AT 17:29Gaurav Sharma
November 28, 2025 AT 17:14Shubham Semwal
November 29, 2025 AT 20:16Sam HardcastleJIV
November 30, 2025 AT 21:52Mira Adam
December 2, 2025 AT 13:12Miriam Lohrum
December 2, 2025 AT 18:45archana das
December 2, 2025 AT 19:51Emma Dovener
December 3, 2025 AT 19:05Sue Haskett
December 3, 2025 AT 22:07Jauregui Goudy
December 5, 2025 AT 03:40Tom Shepherd
December 5, 2025 AT 05:39Rhiana Grob
December 6, 2025 AT 23:05Frances Melendez
December 8, 2025 AT 09:54Jonah Thunderbolt
December 9, 2025 AT 00:06Rebecca Price
December 9, 2025 AT 21:05