TL;DR
- Stuffy nose and watery eyes often signal the same underlying issue.
- Skipping regular eye exams can let serious eye problems hide.
- Eye doctors can spot early signs of infection, allergies, or drainage blockages.
- Schedule an exam if symptoms persist more than a week, after a cold, or during allergy season.
- Simple home habits-hydration, humidifiers, and gentle eye wipes-help both nose and eyes.
How a Blocked Nose and Red, Watery Eyes Are Connected
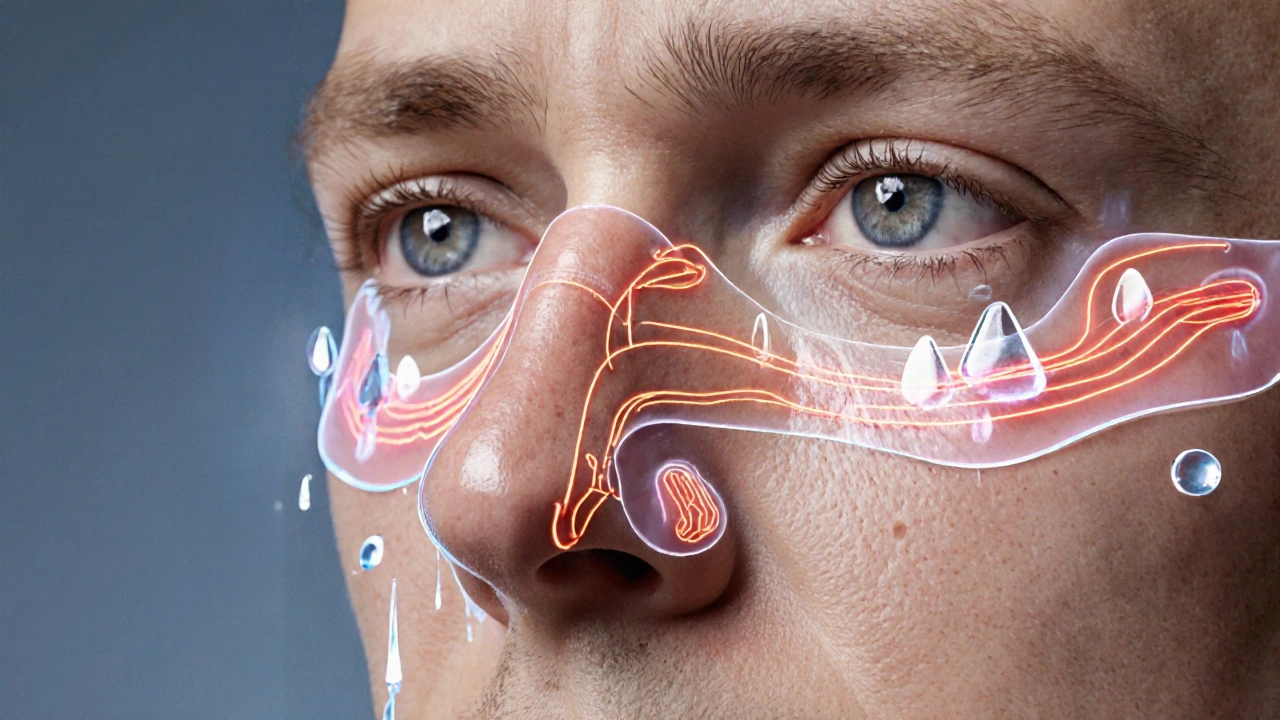
When the nasal passages get clogged, you might notice a sting of tears that seems out of nowhere. The reason is simple anatomy: the eyes and nose share a drainage route called the nasolacrimal duct a tiny channel that carries tears from the eye surface into the nasal cavity. If that duct or the surrounding tissues swell, tears can’t drain properly, so they spill over the lids.
Two common culprits-nasal congestion the feeling of a blocked or stuffy nose, often caused by allergies, colds, or sinus infections and allergic conjunctivitis inflammation of the eye’s surface triggered by airborne allergens-can start a domino effect. Congestion inflames the lining of the sinuses, which in turn irritates the conjunctiva (the eye’s outer membrane). The eye responds by producing extra tears, and the blocked drainage makes those tears look like a constant runny faucet.
Why Skipping Eye Exams Is Risky
It’s easy to think that a runny eye is just a nuisance, especially if you’ve had a cold or allergy flare‑up before. But regular check‑ups catch problems that feel harmless at first. For example, chronic blockage of the nasolacrimal duct can lead to dry eye syndrome a condition where insufficient tear production or poor tear quality damages the eye surface. Paradoxically, too many tears from a blocked duct can dry out the eye’s surface over time.
More serious is the risk of secondary infection. Stagnant fluid behind the eye can become a breeding ground for bacteria, eventually turning a simple irritation into conjunctivitis an infection or inflammation of the conjunctiva that may require antibiotic drops that spreads to other parts of the eye.
Even if you’re otherwise healthy, an eye exam can reveal hidden glaucoma, early cataract formation, or retinal changes that have nothing to do with your nose but can threaten sight if left untreated.
What a Regular Eye Exam Actually Checks
A thorough appointment with an ophthalmologist a medical doctor specialized in eye and vision care, capable of diagnosing and treating eye diseases or an optometrist covers several key areas:
- Visual acuity - how clearly you see at distance and near.
- Refraction - determining the correct prescription for glasses or contacts.
- Eye pressure - a quick tonometry test that screens for glaucoma.
- External inspection - checking lids, lashes, cornea, and the nasolacrimal duct for blockages or inflammation.
- Fundus exam - looking at the retina and optic nerve for signs of disease.
- Colour and contrast testing - assessing how well your eyes process visual information.
During the external inspection, the clinician may use a tiny light or a fluorescein dye to highlight any abnormal tear drainage or surface damage. This quick step often reveals whether your watery eyes are just a symptom of nasal congestion or something deeper.
When Nasal Issues Directly Impact Eye Health
Three scenarios tend to pop up most often:
- Allergic rhinitis + allergic conjunctivitis: Pollen, dust mites, or pet dander trigger a cascade of histamine release that inflames both nasal passages and eye membranes. You’ll get sneezing fits, a runny nose, itchy eyes, and that classic red‑watery look.
- Acute sinus infection (sinusitis): A bacterial or viral infection fills the sinus cavities with mucus, raising pressure on nearby eye structures. The result can be a dull ache behind the eyes, blurry vision, and excessive tearing.
- Chronic nasal polyps: These soft, non‑cancerous growths block airflow and tear drainage for months or years. They often require surgical removal, but until then they keep the eyes perpetually watery.
In each case, an eye exam can differentiate whether the tear production is a protective response or a sign of an emerging eye disorder.
Key Signs It’s Time to Book an Eye Exam
Don’t wait for a full-blown infection before you act. Here are the red flags that should trigger a visit within 7‑10 days:
- Persistent watery eyes that don’t improve after nasal decongestants.
- New discharge that is yellow, green, or thick.
- Eye pain, especially around the brow or behind the ear.
- Blurred vision that comes and goes.
- Noticeable swelling of the eyelids or a feeling of something stuck in the eye.
If you’ve just recovered from a cold but the symptoms linger, consider a quick check‑up. The exam is painless and usually takes under 30 minutes.
Simple Home Strategies to Ease Both Nose and Eyes
While you’re waiting for that appointment, a few everyday tweaks can relieve the discomfort:
- Use a humidifier: Moist air thins nasal mucus and reduces tear over‑production.
- Stay hydrated: Drinking plenty of water keeps the tear film balanced.
- Saline nasal rinse: A Neti pot or squeeze bottle clears out allergens and mucus, easing pressure on the nasolacrimal duct.
- Warm compress on the eyes: A clean, warm washcloth for 5 minutes opens up the tear ducts and soothes irritation.
- Avoid eye‑rubbing: Rubbing can push bacteria deeper and worsen inflammation.
If allergies are the main trigger, an allergy test a skin prick or blood test that identifies specific allergens causing your symptoms can guide long‑term medication or environmental changes.
Comparison Table: Common Causes of Blocked Nose + Watery Eyes
| Condition | Primary Cause | Typical Eye Symptom | When to See a Doctor |
|---|---|---|---|
| Allergic Rhinitis + Conjunctivitis | Seasonal or indoor allergens | Itchy, red, watery eyes | Symptoms > 7 days or severe itching |
| Acute Sinusitis | Viral/bacterial infection | Cloudy vision, pressure‑induced tearing | Fever, facial pain, or worsening after 5 days |
| Nasal Polyps | Chronic inflammation | Constant tearing, nasal blockage | Persistent symptoms > 3 months |
| Dry Eye Syndrome | Insufficient tear quality | Watery eyes after a short‑term dryness | Burning, gritty sensation, blurry vision |
Next Steps After Your Exam
Once the ophthalmologist finishes the assessment, they’ll usually suggest a tailored plan:
- Prescription eye drops: Anti‑histamine or anti‑inflammatory drops for allergy‑related redness.
- Nasal spray: Steroid sprays to reduce sinus swelling, indirectly easing tear drainage.
- Procedural options: If a nasolacrimal duct blockage is severe, a simple in‑office probe can open the channel.
- Follow‑up schedule: Most doctors recommend revisiting every 12 months, or sooner if symptoms flare.
By treating both the nose and the eyes together, you’ll keep the cycle of irritation from looping back on itself.
Frequently Asked Questions
Can a cold really cause my eyes to water?
Yes. A cold inflames the nasal lining, which can block the nasolacrimal duct. The eyes produce extra tears to compensate, leading to that watery look.
Do I need an eye exam if I already have a sinus infection?
It’s wise to get evaluated. A sinus infection can press on eye structures and sometimes cause secondary infections that only an eye doctor can spot early.
What’s the difference between allergic conjunctivitis and a bacterial eye infection?
Allergic conjunctivitis usually brings clear, watery discharge and intense itching, while a bacterial infection produces thick, colored pus and can cause crusting overnight.
Can over‑the‑counter decongestants help my eyes?
They may reduce nasal swelling, which can indirectly improve tear drainage, but they won’t treat the eye surface itself. Pair them with appropriate eye drops if needed.
How often should I get an eye exam if I have chronic allergies?
At least once a year, and sooner if you notice worsening redness, vision changes, or persistent tearing.



 Medications
Medications




Vandita Shukla
September 28, 2025 AT 09:31Skipping your eye exam while you’ve got a blocked nose just buries the problem deeper.
Susan Hayes
October 3, 2025 AT 16:00Look, we’ve got the best eye doctors right here in the States, and they’re not going to wait for you to suffer in silence. When your nasal passages are clogged, your tear ducts get backed up, and that’s a clear sign you need a professional check‑up. Ignoring it isn’t an option – it’ll only worsen and could lead to infection. Trust the system, get that exam scheduled ASAP.
Michael Leaño
October 9, 2025 AT 10:53Hey, I totally get how annoying watery eyes can be, especially when you’re already battling a stuffy nose. A quick visit to the optometrist can pinpoint whether it’s just congestion or something that needs treatment. Don’t let it linger; early detection makes everything easier to fix. You’ve got this!
Anirban Banerjee
October 15, 2025 AT 05:46Inclusive mentorship suggests that patients consider the anatomical link between the nasolacrimal duct and the nasal cavity when evaluating persistent lacrimation. A comprehensive ocular examination not only assesses visual acuity but also inspects the external ocular structures for signs of ductal obstruction. It is prudent to schedule such an evaluation within a week of symptom onset to preempt secondary complications. Should the findings indicate chronic blockage, referral for dacryocystorhinostomy may be warranted.
Ernie Rogers
October 21, 2025 AT 00:40Honestly the whole thing could be solved with a simple decongestant but the US health system wants you to pay for extra tests.
Eunice Suess
October 26, 2025 AT 18:33Listen, you’re not gonna fix that watery mess by just sipping tea – you need proper diagnostics! It’s not like “just a cold” when the tear ducts are clogged. Get checked or you’ll be dealing with a constant drip, like a leaky faucet. Please stop ignoring the signs!
Anoop Choradia
November 1, 2025 AT 13:26It is evident that mainstream ophthalmic guidelines downplay the prevalence of nasolacrimal obstruction in order to conceal pharmaceutical interests. A meticulous review of peer‑reviewed literature reveals a pattern of selective reporting that benefits certain manufacturers. Consequently, an informed patient should seek an independent clinician who adheres strictly to evidence‑based protocols, thereby avoiding potential conflicts of interest.
bhavani pitta
November 7, 2025 AT 08:20While many advocate immediate ophthalmic assessment, it is worth noting that in some cases the edema resolves spontaneously with appropriate nasal irrigation, rendering urgent referral unnecessary.
Brenda Taylor
November 13, 2025 AT 03:13Honestly, you could just keep ignoring the drip and hope it goes away 🙄. Moral of the story: take responsibility for your health before it becomes someone else’s problem.
Dana Sellers
November 18, 2025 AT 22:06People need to stop playing games with their eyes – clean up the mess and get checked.
Damon Farnham
November 24, 2025 AT 17:00Indeed!!! It is absolutely unacceptable that anyone would neglect such a critical health measure!!! The nation's future depends on vigilant citizens!!!
Gary Tynes
November 30, 2025 AT 11:53Yo, just grab a Neti pot, stay hydrated, and swing by your optometrist when you can. It’ll help both the nose and eyes not to freak out.
Marsha Saminathan
December 6, 2025 AT 06:46First off, kudos for taking the initiative to look into this tangled nose‑eye drama!
Your eyes are basically little rivers that rely on a smooth highway to drain into the nose.
When that highway hits traffic due to congestion, the runoff backs up and you end up looking like a leaky faucet.
Now, imagine that backed‑up fluid as a party that invites bacteria without an invitation.
Those unwanted guests can turn a simple irritation into a full‑blown infection faster than you can say 'sneezing'.
That's why a regular eye exam acts like a bouncer, checking IDs and kicking out troublemakers before they crash the venue.
During the exam, the doc will flash a tiny light, maybe sprinkle fluorescein, and watch how your tears roll across the cornea.
If they spot unusual staining or sluggish drainage, they'll recommend a gentle warm compress or even a quick in‑office probe to clear the duct.
Meanwhile, at home, keep the air moist with a humidifier, because dry air is the villain that thickens mucus and clogs pathways.
Don’t forget to stay hydrated-water is the unsung hero that keeps your tear film slick and your sinuses flowing.
A saline rinse once or twice a day can whisk away allergens and excess mucus, giving your nasolacrimal duct a breather.
And yes, you can totally rock stylish glasses while you’re at it; they don’t impede drainage if fitted properly.
If allergies are the main culprit, an antihistamine or a prescription eye drop can calm the storm in both your nose and eyes.
Should symptoms persist beyond a week, book that eye doctor appointment without delay, because early intervention saves you from chronic woes.
In short, treat your nose and eyes as a team, not as isolated strangers, and you’ll keep the watery drama at bay.
Justin Park
December 12, 2025 AT 01:40Isn't it fascinating how the body mirrors the concept of interconnectedness, reminding us that a blocked path in one area reverberates elsewhere? 🌐💧