HIV Treatment – What You Need to Know Today
Living with HIV means staying on the right meds every day. The good news is that modern treatment can keep the virus at bay, protect your immune system and let you lead a normal life. This page breaks down the main drug families, how they work together, and practical steps to make therapy easier.
Core Pillars of HIV Therapy
Most people use a combination called antiretroviral therapy (ART). ART mixes three or more drugs from different classes so the virus can’t find an easy way to grow. The three biggest classes are:
- Integrase inhibitors – stop the virus from inserting its DNA into your cells. Examples: dolutegravir, bictegravir.
- Protease inhibitors – block the enzyme that cuts viral proteins into functional pieces. Examples: darunavir, atazanavir.
- Non‑nucleoside reverse transcriptase inhibitors (NNRTIs) – jam the reverse transcriptase enzyme that copies viral RNA. Examples: efavirenz, rilpivirine.
Many first‑line regimens pair an integrase inhibitor with two nucleoside reverse transcriptase inhibitors (NRTIs) like tenofovir and emtricitabine. This combo is called a “single‑tablet regimen” because you swallow one pill a day.
Choosing the Right Regimen
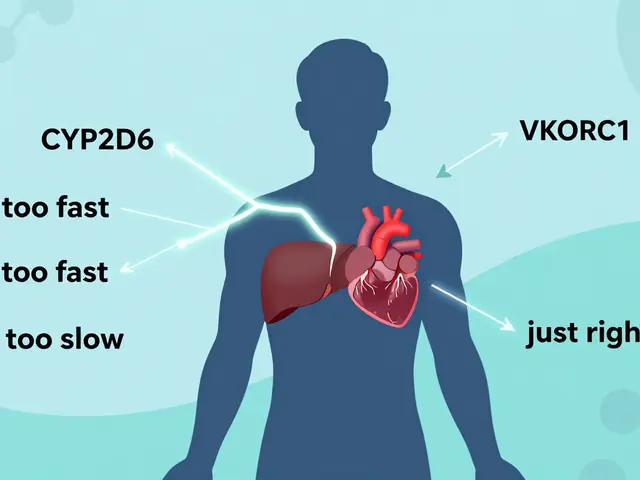
Doctors pick a plan based on your health, other meds, and lifestyle. If you have kidney issues, they’ll avoid tenofovir disoproxil fumarate and may use tenofovir alafenamide instead. If you’re pregnant, certain drugs are safer – usually dolutegravir after the first trimester, or boosted protease inhibitors.
Side‑effects vary. Some people feel nausea with NNRTIs, while integrase inhibitors can cause mild weight gain. Talking to your provider about any new symptom helps adjust the regimen before problems get worse.
Adherence is the biggest factor in success. Missing doses lets the virus rebound and can cause resistance. Set a daily alarm, keep pills in a visible spot, or use a pill‑box with compartments for each day. If you travel, pack enough meds for the whole trip plus a few extra in case of delays.
Regular lab checks track how well the treatment works. A viral load under 50 copies/ml means the virus is suppressed. CD4 counts over 500 cells/mm³ usually indicate a healthy immune system. Most doctors schedule these tests every three to six months.
New drugs keep coming out. Long‑acting injectables like cabotegravir plus rilpivirine can be given every two months, which is great for people who don’t want daily pills. Keep an eye on FDA updates or ask your clinician if a newer option fits your needs.
Finally, remember that treatment isn’t just about pills. Eating a balanced diet, staying active, and managing stress all support immune health. If you feel isolated, look for local support groups or online communities – sharing experiences makes the journey less lonely.
With the right regimen, regular monitoring, and a bit of routine, HIV can stay under control. Talk to your healthcare team, ask questions, and stick to the plan that works best for you.
This article digs deep into the cost-effectiveness of lamivudine in managing HIV and hepatitis B. It explores how lamivudine compares to other treatments in price and results, provides useful data, and highlights practical tips for patients and caregivers. You'll find authentic facts, recent studies, and insights on real-life impacts for both individuals and health systems. The article is packed with hands-on information for those navigating long-term antiviral therapy.



 Medications
Medications
![Buy Generic Zovirax (Acyclovir) Online Cheap in the UK [2025]: Safe, Legal, and Fast](/uploads/2025/08/thumbnail-buy-generic-zovirax-acyclovir-online-cheap-in-the-uk-2025-safe-legal-and-fast.webp)