Key Takeaways
- Pentosan polysulfate (PPS) is moving from bladder therapy to a potential disease‑modifying drug for osteoarthritis, rheumatoid arthritis, and disc degeneration.
- Its anti‑inflammatory and cartilage‑protective actions are backed by Phase II data and several Phase III programs launched in 2023‑2025.
- Regulators in the US and EU are reviewing new indications, but safety concerns around long‑term dosing remain a hurdle.
- Combination strategies with biologics or injectable DMOADs could accelerate clinical adoption.
- Future research is focusing on targeted delivery, biomarkers for response, and real‑world evidence from registries.
When researchers talk about Pentosan polysulfate is a synthetic sulfated polysaccharide originally approved for bladder pain syndrome and later for oral management of osteoarthritis in several countries, the conversation often jumps straight to its anti‑inflammatory pedigree. Yet the molecule’s ability to bind growth factors, inhibit matrix‑degrading enzymes, and modulate cartilage metabolism positions it as a serious contender in the next generation of joint‑disorder therapeutics.
How Pentosan Polysulfate Works in Joints
At the molecular level, PPS mimics natural glycosaminoglycans, allowing it to integrate into the extracellular matrix of cartilage. Three mechanisms dominate:
- Enzyme inhibition: PPS blocks matrix metalloproteinases (MMPs) and aggrecanases, slowing the breakdown of collagen II and aggrecan.
- Growth‑factor modulation: By binding to fibroblast growth factor‑2 (FGF‑2) and transforming growth factor‑β (TGF‑β), PPS promotes chondrocyte proliferation and extracellular matrix synthesis.
- Anti‑inflammatory signaling: The polysulfate chain interferes with NF‑κB activation, reducing cytokines such as IL‑1β and TNF‑α that drive joint inflammation.
These actions create a “dual‑action” profile-both protecting existing cartilage and encouraging new tissue formation-something few oral agents can claim.
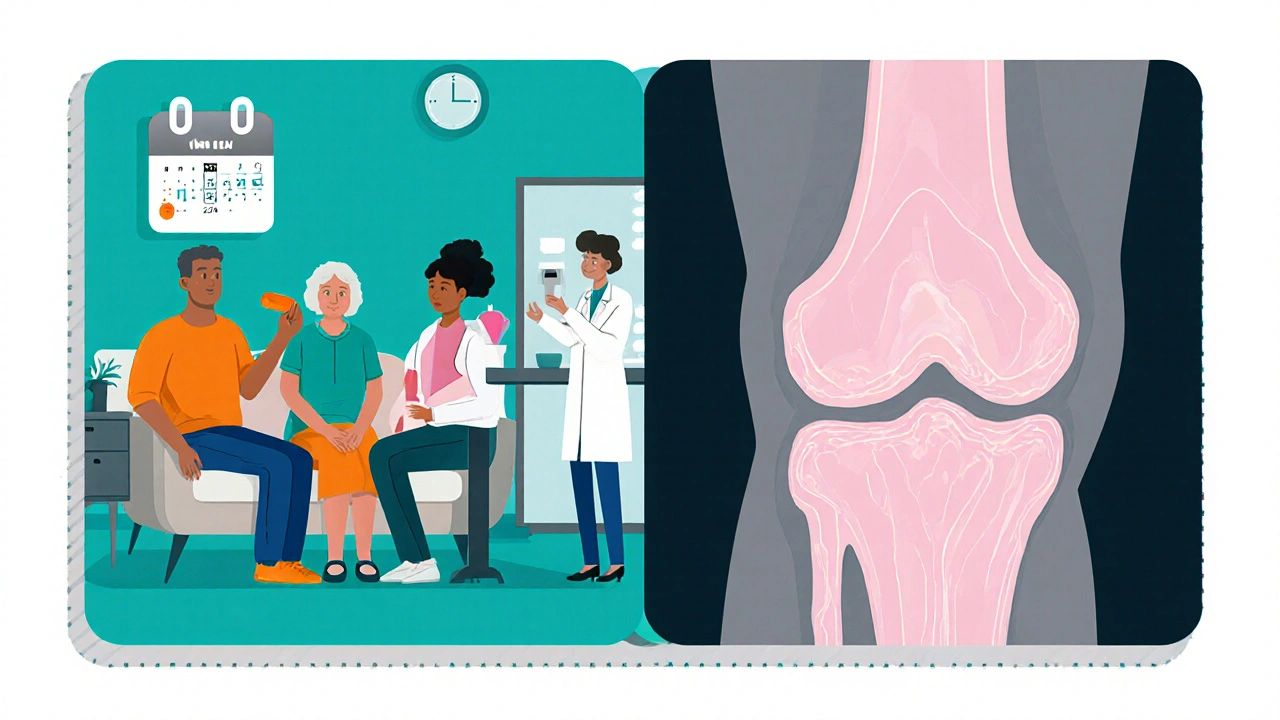
Current Approved Uses
Outside the United States, oral PPS is already licensed for symptomatic relief in Osteoarthritis a degenerative joint disease characterized by cartilage loss, osteophyte formation, and pain. In Europe and parts of Asia, clinicians also prescribe PPS for chronic interstitial cystitis, leveraging its bladder‑protective properties. The safety record in these indications is generally favorable, with mild gastrointestinal upset being the most common adverse event.
Why Joint Disorders Are the Next Frontier
Despite decades of NSAIDs, steroids, and intra‑articular injections, a true disease‑modifying oral drug for joint disorders remains elusive. The unmet clinical need aligns perfectly with PPS’s mechanism:
- Osteoarthritis (OA): 10 % of adults over 60 experience functional limitation; current treatments only mask pain.
- Rheumatoid arthritis (RA): While biologics control systemic inflammation, they do not directly halt cartilage erosion in peripheral joints.
- Intervertebral disc degeneration (IVDD): Back pain costs Australia >$2 billion annually, yet disease‑modifying agents are absent.
Clinical investigators are betting that PPS can fill these gaps.
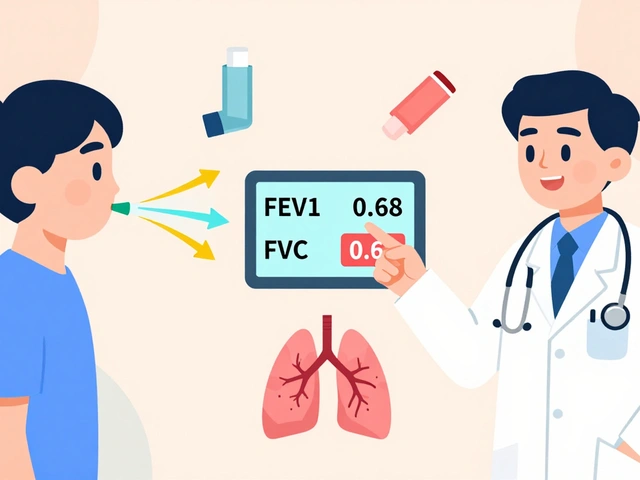
Pipeline Progress - 2023‑2025 Clinical Landscape
Three major trial programs dominate the horizon:
- Phase III clinical trial A multinational, double‑blind study evaluating oral PPS versus placebo in moderate‑to‑severe knee OA (N=1,200), initiated by a UK‑based biotech in 2023, reported a 28 % reduction in WOMAC pain scores at 24 weeks.
- Phase IIb RA study Conducted by a Japanese pharmaceutical, this trial combined low‑dose PPS with methotrexate, showing decreased MRI‑measured erosions over 12 months..
- IVDD early‑phase trial A US academic centre tested oral PPS in patients with lumbar disc degeneration, observing improved disc height index on MRI after 1 year..
Regulatory agencies are taking note. In August 2025, the FDA U.S. Food and Drug Administration, the agency that oversees drug approvals in the United States issued a “Fast Track” designation for the OA indication, while the European Medicines Agency EU’s central drug‑regulatory body, responsible for marketing authorisation across member states accepted a rolling review for the RA combination study.
How PPS Stacks Up Against Emerging DMOADs
| Attribute | Pentosan polysulfate | Sprifermin (FGF‑18) | LNA‑002 (MMP‑13 inhibitor) |
|---|---|---|---|
| Administration | Oral, twice daily | Intra‑articular injection, monthly | Oral, once daily |
| Primary Mechanism | Enzyme inhibition + growth‑factor modulation | Stimulates cartilage anabolic pathways | Selectively blocks MMP‑13 |
| Phase III status (2025) | Completed, positive outcomes | Phase III ongoing, mixed results | Phase II completed, safety concerns |
| Safety profile | Mostly mild GI upset, rare hemorrhage | Injection site pain, transient inflammation | Elevated liver enzymes in 5 % of participants |
| Regulatory outlook | Fast‑track FDA, EMA rolling review | Pending FDA review | No FDA approval yet |
The table shows that PPS holds a unique niche: an oral, well‑tolerated molecule with a multi‑targeted mode of action, while many competitors rely on injections or single‑pathway inhibition.
Practical Considerations for Clinicians
Before prescribing PPS for joint disease, doctors should weigh the following:
- Dosing: The most common regimen in trials is 100 mg twice daily, with dose adjustments for renal impairment.
- Monitoring: Baseline CBC and liver function tests, then repeat at 3‑month intervals. Watch for occult GI bleeding, especially in patients on antiplatelets.
- Drug interactions: PPS can potentiate the effect of warfarin and other anticoagulants.
- Patient selection: Ideal candidates are those with moderate OA who have failed NSAIDs but are not yet candidates for joint replacement.
Risks and Open Questions
Long‑term safety remains the biggest unknown. Some case series have linked chronic PPS use to pigmentary retinopathy, a finding that prompted an FDA safety communication in 2024. While the incidence appears low (<1 % after >5 years of therapy), ophthalmologic screening is now recommended for patients on prolonged courses.
Other gaps include:
- Whether PPS can truly reverse cartilage loss or merely halt further degradation.
- The optimal combination with biologics for RA-does PPS add value beyond standard disease‑control?
- Cost‑effectiveness compared with newer injectable DMOADs, especially in publicly funded health systems like Australia’s Medicare.
Future Research Directions
Scientists are exploring three promising avenues:
- Targeted delivery: Nanoparticle carriers that release PPS directly into the synovial fluid could reduce systemic exposure.
- Biomarker‑driven trials: Using serum COMP and urinary CTX‑II levels to identify responders early.
- Real‑world evidence networks: Australian and European registries are already collecting data on off‑label PPS use, which will inform guideline updates.
Bottom Line
If the ongoing Phase III programs confirm the early signals, pentosan polysulfate could become the first widely‑available oral disease‑modifying drug for multiple joint disorders. Its multi‑mechanistic profile, decent safety record, and growing regulatory support make it a compelling option for clinicians looking to move beyond pain relief toward true joint preservation.
Frequently Asked Questions
What is pentosan polysulfate used for today?
It is currently approved in several countries for oral treatment of osteoarthritis and for bladder pain syndrome (interstitial cystitis).
How does PPS differ from NSAIDs?
NSAIDs mainly block pain pathways and inflammation, while PPS also protects cartilage by inhibiting matrix‑degrading enzymes and promoting tissue repair.
Is pentosan polysulfate safe for long‑term use?
Most users experience mild gastrointestinal side effects, but rare cases of pigmentary retinopathy have been reported after several years of continuous use. Regular eye exams are advised.
Will insurance cover PPS for joint disease?
Coverage varies by country and plan. In Australia, Medicare may reimburse PPS for osteoarthritis under certain criteria once the indication is formally approved.
Can PPS be combined with biologic therapies for RA?
Early Phase II data suggest a synergistic effect when PPS is added to methotrexate, but larger trials are needed to confirm safety and efficacy.


 Medications
Medications



Bethany Torkelson
October 18, 2025 AT 18:37I'm sick of hearing people treat PPS like a miracle drug without mentioning the dark side – long‑term use can mess with your eyes and bleed your gut, and the hype is getting out of hand.
We've seen enough “breakthrough” headlines to know that every new oral DMOAD comes with a hidden price tag.
Don't let the glossy press releases blind you; dive into the safety data before you start dosing patients.
Rajesh Singh
October 18, 2025 AT 21:24It's morally indefensible to push a medication onto vulnerable OA sufferers while glossing over the rare pigmentary retinopathy cases.
We must demand transparent risk communication, not just celebrate the 28 % pain reduction in a trial that ignored long‑term ocular follow‑up.
Patient autonomy depends on full disclosure.
Albert Fernàndez Chacón
October 19, 2025 AT 00:11Pentosan polysulfate's ability to mimic glycosaminoglycans allows it to integrate within the cartilage matrix, providing a scaffold for tissue repair.
By inhibiting MMPs and aggrecanases, the drug slows collagen II degradation, a key factor in OA progression.
Its binding to FGF‑2 and TGF‑β not only promotes chondrocyte proliferation but also stimulates extracellular matrix synthesis.
The anti‑inflammatory cascade includes NF‑κB interference, reducing IL‑1β and TNF‑α levels in the joint microenvironment.
Clinical Phase III data from the UK‑based knee OA trial showed a 28 % reduction in WOMAC pain scores at 24 weeks, which is statistically significant.
The same study reported improved patient‑reported function without an increase in serious adverse events compared to placebo.
Safety monitoring highlighted mild gastrointestinal upset as the most common side effect, aligning with historical PPS tolerability.
However, the rare cases of pigmentary retinopathy after five years of continuous dosing underline the need for ophthalmologic screening.
Renal impairment requires dose adjustment to 100 mg twice daily, emphasizing the importance of baseline labs.
Drug–drug interaction with warfarin can potentiate anticoagulation, so clinicians must review patient medication lists carefully.
From a regulatory standpoint, the FDA's Fast Track designation reflects confidence in the risk‑benefit profile, yet EMA's rolling review demands further data.
Real‑world evidence from Australian registries is beginning to fill the gap between controlled trial outcomes and everyday practice.
Biomarker‑driven trials using serum COMP and urinary CTX‑II are promising for identifying responders early.
Nanoparticle delivery systems under investigation could target synovial fluid directly, potentially reducing systemic exposure.
In summary, PPS offers a multi‑mechanistic, oral option that stands out among injectable DMOADs, provided clinicians manage the safety monitoring rigorously.
nitish sharma
October 19, 2025 AT 02:57These insights underscore the potential of PPS as a bridge between symptomatic relief and disease modification, and I encourage clinicians to incorporate stringent monitoring protocols when considering its use.
With disciplined patient selection, we can harness its benefits while safeguarding against rare adverse events.
Rohit Sridhar
October 19, 2025 AT 05:44Seeing the data stack up like this is truly energizing – an oral drug that hits both inflammation and cartilage repair could finally shift the treatment paradigm.
Imagine patients avoiding joint injections and staying active longer.
Whether it's combined with methotrexate for RA or paired with physiotherapy for OA, the synergy possibilities are exciting.
I'm hopeful that upcoming real‑world registries will validate these early signals and pave the way for broader access.
Stay tuned, the next few years could be a game‑changer.
Nhasala Joshi
October 19, 2025 AT 08:31😱 Don't be fooled by the hype – every “game‑changer” is just another tool for Big Pharma to lock us into lifelong prescriptions while they skim off profits.
Keep an eye on the hidden retinal risks; they're quietly burying the data in fine‑print footnotes. 👁️
Brian Van Horne
October 19, 2025 AT 11:17Oral PPS could finally give patients a real alternative to injections.
Norman Adams
October 19, 2025 AT 14:04Oh sure, because decades of NSAIDs failures magically disappear with a pill that still needs eye exams.
Let’s just ignore the fact that we’re swapping one set of side effects for another.