Bronchial Asthma vs COPD Diagnosis Helper
This tool helps distinguish between bronchial asthma and COPD by evaluating key clinical features. Select the options that best match the patient's profile.
Select the patient's features and click "Diagnose Condition" to see the differential diagnosis.
Quick Takeaways
- Bronchial asthma usually starts in childhood, while COPD appears in adulthood, often after years of smoking.
- Asthma symptoms are highly reversible with medication; COPD changes are only partially reversible.
- Spirometry is the common test, but doctors look for different patterns to tell them apart.
- Inhaled corticosteroids are a mainstay for asthma; bronchodilators and lifestyle changes dominate COPD care.
- Both need an action plan, but triggers and long‑term strategies differ.
What Are Bronchial Asthma and COPD?
When you hear the words bronchial asthma is a chronic inflammatory disease of the airways that causes episodes of wheezing, breathlessness, chest tightness and coughing, picture a set of tubes that swell and tighten whenever a trigger shows up - pollen, dust, cold air, or stress. The inflammation is driven by an overactive immune response, and the narrowing can often be undone with a quick‑acting inhaler.
In contrast, COPD (chronic obstructive pulmonary disease) is a progressive lung disorder marked by persistent airflow limitation, usually caused by long‑term exposure to irritants like tobacco smoke. COPD groups two main problems - chronic bronchitis (thick mucus lining the airways) and emphysema (damage to the tiny air sacs). Both shrink the lungs' ability to move air in and out, and the changes are only partly reversible.
Key Differences at a Glance
| Aspect | Bronchial Asthma | COPD |
|---|---|---|
| Typical Onset | Childhood or early adulthood | Usually after age 40 |
| Main Cause | Allergic or non‑allergic triggers; genetics | Long‑term smoke exposure; occupational dust |
| Airway Changes | Reversible bronchoconstriction, eosinophilic inflammation | Irreversible airway narrowing, mucus hypersecretion, alveolar destruction |
| Reversibility (spirometry) | >12% improvement after bronchodilator | <12% improvement; fixed obstruction |
| Typical Symptoms | Intermittent wheeze, night‑time cough, trigger‑related attacks | Persistent cough with sputum, dyspnea on exertion, chest tightness |
| First‑line Treatment | Inhaled corticosteroids + quick‑relief bronchodilator | Long‑acting bronchodilators, smoking cessation, pulmonary rehab |

How Symptoms Show Up Differently
Both conditions make you feel short of breath, but the pattern tells a story. Asthma often flares up suddenly - you might notice a tickle in your throat after mowing the lawn, then within minutes you’re reaching for your reliever inhaler. The relief is fast, and you can usually return to normal activities.
COPD, on the other hand, brings a slow, steady climb in breathlessness. You may develop a chronic cough that produces mucus every morning, and climbing a few steps can leave you winded for a long time. The symptoms linger even after resting, reflecting permanent airway damage.
Diagnosing the Two: What Spirometry Reveals
Spirometry is a breathing test that measures the volume of air you can exhale forcefully and how quickly you can do it. Doctors use it to see how much the airways can open after a bronchodilator.
In asthma, the post‑bronchodilator FEV1 (forced expiratory volume in 1 second) jumps noticeably - usually more than a 12% and 200ml increase. COPD shows a modest or no jump, confirming a fixed obstruction.
Sometimes a chest X‑ray or CT scan is ordered to spot emphysema‑related “holes” in the lungs, or blood tests check for eosinophils, which are higher in many asthma patients.
Managing Each Condition Effectively
Even though both diseases use inhalers, the drug mix varies.
- Inhaled corticosteroids are anti‑inflammatory medicines that keep asthma airway swelling low. They’re taken daily, not just during attacks.
- For COPD, bronchodilators (LABA or LAMA) are the backbone, opening the narrowed tubes for longer periods.
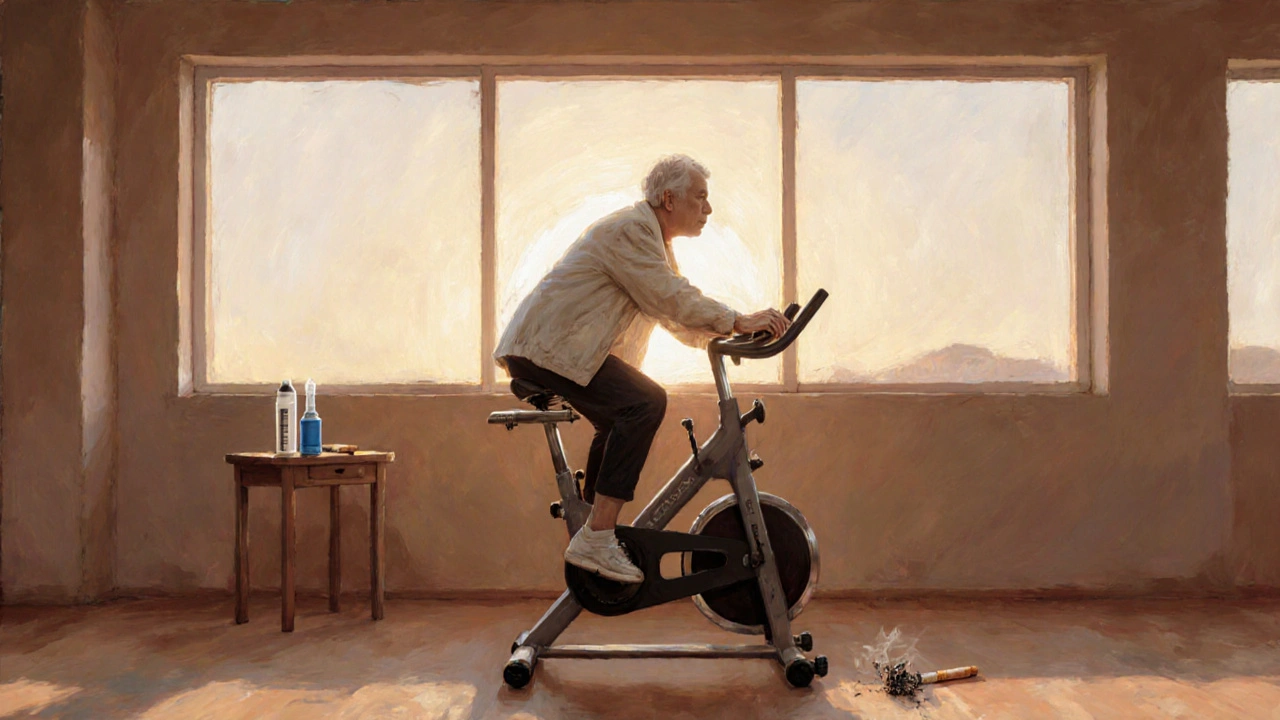
- Smoking cessation is the single most powerful step for COPD; even cutting back can slow lung decline.
- Asthma patients benefit from an action plan that outlines when to use a rescue inhaler versus stepping up to steroids.
- COPD patients often join pulmonary rehabilitation - a structured exercise and education program that improves stamina.
Quick Checklist for Patients
- Know your trigger list - pollen, pet dander, cold air for asthma; avoid smoke and dust for COPD.
- Carry a reliever inhaler at all times if you have asthma; keep long‑acting inhalers handy for COPD.
- Schedule regular spirometry - at least once a year for asthma, every 1‑2 years for COPD.
- Track symptoms in a diary - note when breathlessness starts, its duration, and any medication used.
- Discuss vaccination (flu, pneumococcal) with your doctor; both conditions raise infection risk.
Common Misconceptions Debunked
Misconception 1: “If I have asthma, I can’t develop COPD.” Not true. A long history of smoking can lead to COPD even in asthmatics, creating an overlap syndrome.
Misconception 2: “COPD always means you’ll need oxygen.” Only severe stages (GOLD3‑4) require supplemental oxygen; many manage well with inhalers and lifestyle changes.
Misconception 3: “Asthma is only a childhood disease.” Adult‑onset asthma accounts for about 20% of cases and often mimics COPD, so clear diagnosis matters.
When to Seek Medical Help Immediately
If you notice any of these red flags, call emergency services or go to the nearest A&E:
- Sudden, severe chest tightness that doesn’t improve with a rescue inhaler.
- Blue‑tinged lips or fingertips (sign of low oxygen).
- Rapid breathing (>30 breaths per minute) or inability to speak full sentences.
- Confusion, dizziness, or fainting.
For milder worsening - like an increase in night‑time coughing or a need for more frequent reliever use - contact your GP promptly to adjust the treatment plan.
Frequently Asked Questions
Can asthma turn into COPD?
Asthma itself doesn’t become COPD, but long‑term exposure to smoke or pollutants can cause COPD on top of asthma, creating an overlap condition that needs both anti‑inflammatory and bronchodilator therapy.
Why does my doctor use a bronchodilator test?
The bronchodilator test shows how much your airway can open after medication. A big jump points to asthma; a small or no change suggests COPD.
Are inhaled steroids safe for long‑term use?
When used at the prescribed dose, inhaled corticosteroids are very safe and dramatically lower asthma attacks. Regular monitoring keeps side‑effects, like hoarseness, to a minimum.
What lifestyle changes help COPD patients?
Quitting smoking is the most powerful step. Adding regular low‑impact exercise, a balanced diet, and vaccinations also slow disease progression.
Can children get COPD?
COPD is extremely rare in children because it develops from decades of exposure to irritants. However, children with severe asthma can have airway changes that look like early COPD if they smoke later in life.



 Medications
Medications



McKenna Baldock
October 6, 2025 AT 15:16Understanding the distinction between bronchial asthma and COPD is essential for both clinicians and patients alike. Asthma typically presents early in life, often before the age of 40, and is characterized by reversible airway obstruction. In contrast, COPD usually develops later, frequently in individuals over 40 with a significant smoking history. The diagnostic bronchodilator test provides a clear quantitative measure: an improvement greater than 12 percent suggests asthma, whereas a lower or absent response points toward COPD. Symptom patterns also differ; asthma attacks can be intermittent and triggered by allergens or exercise, while COPD symptoms tend to be persistent and worsen with infections. Recognizing these patterns helps tailor medication strategies, such as the use of inhaled corticosteroids for asthma and bronchodilators for COPD. It also informs lifestyle recommendations, especially smoking cessation for COPD patients. Moreover, the existence of an overlap syndrome means that some patients may exhibit features of both conditions, necessitating a nuanced therapeutic approach. Educational tools that guide patients through these key differences can improve adherence and outcomes. Clinicians should also be aware of comorbidities that can obscure the clinical picture, such as heart failure or obesity. Regular monitoring of lung function allows for early detection of disease progression. Patients with asthma should be encouraged to maintain an action plan for acute exacerbations. Those with COPD benefit from pulmonary rehabilitation programs that include exercise and nutrition counseling. Vaccinations against influenza and pneumococcus are preventative measures that reduce exacerbation risk. Ultimately, a personalized assessment that incorporates age, smoking history, symptom variability, and reversibility testing yields the most accurate diagnosis. By applying these principles, the medical community can better differentiate asthma from COPD and provide optimal care.
Roger Wing
October 7, 2025 AT 19:03This so‑called “tool” is just a gimmick to push pharma profits.
Matt Cress
October 7, 2025 AT 19:05Oh sure because a web widget totally decides your health, right? The whole “pick a box” gimmick is what sci‑fi movies warned us about, defiantly accurate as always. Maybe next they’ll ask us to spin a wheel for a diagnosis of ashtma.
Andy Williams
October 8, 2025 AT 22:50The article correctly outlines the clinical criteria, yet it could benefit from clearer section headings and consistent use of bullet points for readability.
Paige Crippen
October 8, 2025 AT 22:51It’s worth noting that the data sources behind those criteria might be influenced by hidden agendas from big pharma, so we should stay skeptical about the recommendations.
sweta siddu
October 10, 2025 AT 02:36Great breakdown! 😊 This really helps me differentiate the two conditions, especially the part about reversibility after bronchodilators. Thanks for making it so clear!
Ted Mann
October 10, 2025 AT 02:38While the summary is nice, remember that many studies are funded by pharmaceutical companies, which could bias the emphasis on inhaled steroids over lifestyle changes.
Brennan Loveless
October 11, 2025 AT 06:23Honestly, the whole “American healthcare” narrative is overblown; people here have always managed their lungs without fancy tests, so this tool is just another excuse for more bureaucracy.
Vani Prasanth
October 11, 2025 AT 06:25Let’s stay respectful – while it’s true that many patients adapt well, evidence shows early detection and proper management improve quality of life, so tools like this can be valuable when used wisely.
Maggie Hewitt
October 12, 2025 AT 10:10Wow, because we all needed another checklist to tell us what we already know about breathing problems.
Mike Brindisi
October 12, 2025 AT 10:11Honestly the checklist could replace doctors altogether its that simple