Autoimmune Treatments: What Works and How to Choose
If you’ve been told you have an autoimmune condition, the first thing you’ll hear is that treatment can feel like a maze. The good news? There are clear paths you can follow. Below we break down the most common medicines, the newer biologics, and the everyday habits that can make a real difference.
Prescription Options You Should Know
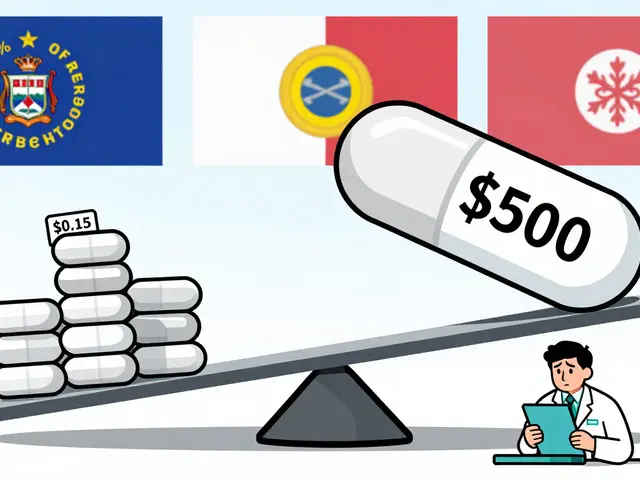
Most doctors start with immunosuppressants – pills that dial down an over‑active immune system. Classic examples include methotrexate, azathioprine, and mycophenolate. They’re cheap, widely studied, and work for diseases like rheumatoid arthritis, lupus, and inflammatory bowel disease.
When a standard immunosuppressant isn’t enough, biologic therapy steps in. Biologics are lab‑engineered proteins that target specific immune pathways. Think of them as smart missiles that zero in on the troublemakers without blowing up the whole army. Popular brands are Humira (adalimumab), Enbrel (etanercept), and Stelara (ustekinumab). They often produce faster relief, but they’re pricier and require regular injections or infusions.
Don’t overlook small‑molecule drugs like JAK inhibitors (tofacitinib, upadacitinib). They sit somewhere between a pill and a biologic, blocking signals that fuel inflammation. For many patients they’re a convenient oral option with solid results.
Regardless of which drug you start, regular blood work is a must. Doctors watch liver enzymes, kidney function, and blood counts to catch side effects early. If you notice new rashes, unusual bruising, or persistent infections, call your prescriber right away.
Lifestyle and Natural Approaches
Medicine isn’t the only tool in the kit. A few everyday habits can boost the effect of your prescription and sometimes let you lower the dose.
Diet matters. Cutting down on processed sugars and fried foods can calm inflammation. Many patients find a Mediterranean‑style diet – lots of olive oil, fish, nuts, and fresh veggies – helps reduce flare‑ups. Some also try an autoimmune protocol (AIP) that eliminates grains, dairy, and nightshades for a few weeks to see if symptoms improve.
Movement is key. Light‑to‑moderate exercise, like walking, swimming, or yoga, keeps joints flexible and releases endorphins that naturally dampen pain. Aim for 30 minutes most days, but listen to your body on bad days – rest when you need it.
Stress management. Chronic stress spikes cortisol, which can trigger immune spikes. Techniques such as deep‑breathing, meditation, or even a short daily walk can lower stress hormones and keep flare‑ups at bay.
Sleep. Quality sleep restores immune balance. Try to get 7‑9 hours, keep the bedroom dark, and avoid screens an hour before bedtime. If you struggle with insomnia, talk to your doctor – sometimes a low‑dose melatonin or sleep‑friendly medication can help.
Lastly, keep a simple symptom journal. Jot down what you ate, how you felt, and any medication changes. Over weeks you’ll spot patterns that point to triggers you can avoid.
Autoimmune treatments combine prescription power with everyday choices. By understanding your meds, staying on top of labs, and supporting your body with diet, movement, and stress control, you can push back against flare‑ups and live a steadier life. Talk to your healthcare team about which options fit your lifestyle – the right mix is often a personal recipe, not a one‑size‑fits‑all solution.
Prednisone isn’t always the best fit for everyone, especially if side effects get in the way. In 2025, you’ve got more choices than ever—meds that work differently and can sometimes mean fewer headaches (literally and figuratively). This article breaks down eight alternatives, giving honest pros, cons, and what you’ll want to ask your doctor. No stuffy jargon, just practical facts to help you partner in your care. Find out what’s new, what works, and what you should know before making a change.



 Medications
Medications