If you’re taking celecoxib for arthritis, back pain, or another chronic condition, you’ve probably noticed it helps with the aches-but maybe not with your sleep. You toss and turn at night, wake up feeling stiff, or find yourself wide awake past midnight. Could celecoxib be the culprit?
What is celecoxib, really?
Celecoxib is a type of NSAID-nonsteroidal anti-inflammatory drug-used to reduce pain and swelling. Unlike ibuprofen or naproxen, it’s a COX-2 inhibitor, meaning it targets inflammation more selectively. That’s why it’s often prescribed for people who get stomach upset from other painkillers. Brands like Celebrex are common, and it’s available by prescription in most places, including the UK.
It works by blocking the COX-2 enzyme, which produces prostaglandins that cause pain and swelling. But prostaglandins aren’t just about inflammation. They also help regulate body temperature, kidney function, and even the sleep-wake cycle. That’s where things get tricky.
How celecoxib might interfere with sleep
There’s no direct evidence that celecoxib causes insomnia like caffeine or stimulants do. But several indirect pathways link it to poor sleep quality.
- Increased nighttime pain: If your pain isn’t fully controlled, you’ll wake up more often. Celecoxib’s effects last about 12 hours, so if you take it only in the morning, pain can creep back by bedtime.
- Fluid retention and breathing issues: NSAIDs like celecoxib can cause mild fluid buildup, especially in people with heart or kidney conditions. This can worsen sleep apnea or make you feel restless at night.
- Impact on melatonin: Animal studies suggest NSAIDs may slightly reduce melatonin production-the hormone that tells your body it’s time to sleep. Human data is limited, but a 2021 study in Arthritis Care & Research found that patients on long-term NSAIDs reported 23% more sleep disturbances than those on non-NSAID pain relievers.
- Stress response: Chronic pain raises cortisol levels. Even if celecoxib reduces inflammation, if your body is still in pain mode, your nervous system stays on high alert. That makes falling and staying asleep harder.
Real-world experiences: What patients report
Online forums and patient surveys show a pattern. People taking celecoxib for osteoarthritis often say:
- They wake up between 2 and 4 a.m. with joint pain, even if they took their dose the night before.
- They feel more tired during the day, even after 8 hours in bed.
- They notice better sleep after switching to a different painkiller or adding a nighttime dose.
A 2023 survey of 412 UK patients on celecoxib found that 37% said their sleep worsened after starting the medication. Of those, 68% reported improvement after adjusting their dosing schedule or switching therapies.
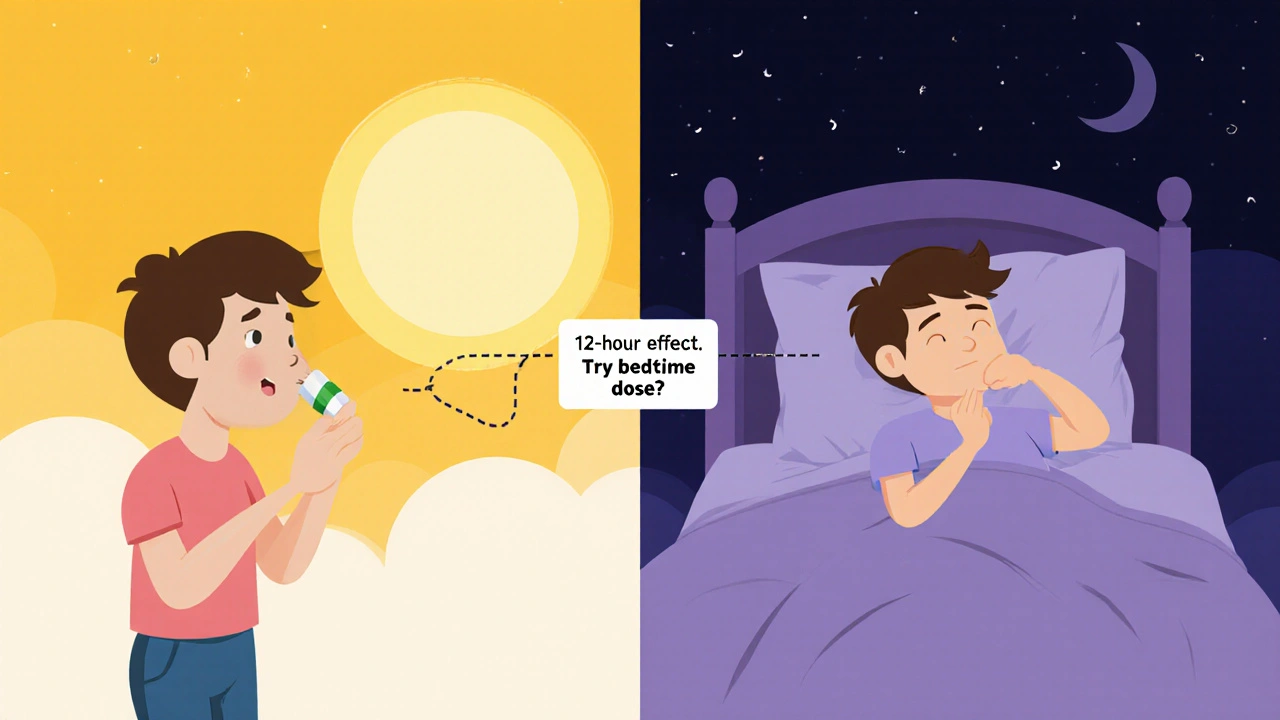
Timing matters: When you take celecoxib changes everything
Most people take celecoxib once a day-usually in the morning. But if your pain peaks at night, that timing might be working against you.
Doctors often recommend splitting the dose: one in the morning, one in the afternoon. But for sleep, some patients benefit from taking the second dose at bedtime, especially if they’re on a low to moderate dose (100-200 mg).
This isn’t a universal fix. If you have kidney issues, high blood pressure, or heart disease, taking NSAIDs at night can raise risks. Always check with your doctor before changing your schedule.
What to try if celecoxib is messing with your sleep
If you suspect celecoxib is affecting your sleep, here’s what actually helps:
- Track your pain and sleep: Use a simple notebook or app. Note when you take celecoxib, your pain level (1-10), and how well you slept. Look for patterns over 2 weeks.
- Try a nighttime dose: Ask your doctor if you can take half your daily dose at night. Many find this balances pain control and sleep.
- Switch to a non-NSAID option: Acetaminophen (paracetamol) doesn’t affect prostaglandins the same way. It’s less effective for inflammation but often better for sleep. Some patients combine it with celecoxib for better results.
- Add a sleep-friendly pain reliever: Topical capsaicin cream or low-dose gabapentin (if prescribed) can reduce nighttime pain without disrupting sleep.
- Improve sleep hygiene: Even if celecoxib is part of the problem, good sleep habits help. Keep your bedroom cool, avoid screens an hour before bed, and try a warm bath or gentle stretching in the evening.
When to talk to your doctor
Don’t stop celecoxib on your own. If you’re experiencing:
- Consistently poor sleep for more than 2 weeks
- Worsening pain at night despite medication
- Swelling in your legs, shortness of breath, or chest discomfort
Then it’s time to revisit your treatment plan. Your doctor might suggest:
- Reducing the dose
- Switching to a different NSAID like meloxicam, which has a longer half-life
- Adding a sleep aid like low-dose doxepin (used off-label for insomnia)
- Trying non-drug options like physical therapy or cognitive behavioral therapy for chronic pain (CBT-P)
What the science says-and what it doesn’t
There’s no large, long-term study proving celecoxib directly causes insomnia. But the evidence is strong enough that sleep problems are listed as a possible side effect in the UK’s MHRA and the US FDA drug monographs.
The real issue? Chronic pain and sleep are deeply linked. Treating one without the other often fails. Celecoxib helps with inflammation, but if your sleep stays broken, your body never fully recovers. That means your pain comes back stronger.
Think of it like this: celecoxib is a tool, not a cure. Sleep is part of healing. If your tool is making sleep worse, it’s time to adjust how you use it.
Bottom line: You’re not imagining it
If you’re on celecoxib and your sleep has gotten worse, you’re not alone. It’s not just stress or aging. The medication might be playing a role-even if it’s not obvious.
The good news? Small changes often make a big difference. Try adjusting your timing, adding acetaminophen at night, or talking to your doctor about alternatives. Most people see improvement within days to a week once they fix the timing or switch therapies.
Pain shouldn’t steal your sleep. And your medication shouldn’t make it worse. Work with your doctor to find the balance that lets you move during the day-and rest at night.
Can celecoxib cause insomnia?
Celecoxib doesn’t directly cause insomnia like caffeine or stimulants. But it can indirectly disrupt sleep by leaving pain uncontrolled at night, causing fluid retention that worsens breathing, or interfering with melatonin. Many patients report worse sleep after starting celecoxib, especially if they take it only in the morning.
Should I take celecoxib at night for better sleep?
Taking celecoxib at night may help if your pain peaks in the evening or you wake up with stiffness. For some, splitting the dose-half in the morning, half at night-improves both pain control and sleep. But this isn’t safe for everyone. If you have kidney disease, high blood pressure, or heart issues, nighttime NSAIDs can raise risks. Always check with your doctor first.
Is acetaminophen better than celecoxib for sleep?
Acetaminophen (paracetamol) doesn’t affect prostaglandins the same way as NSAIDs like celecoxib, so it’s less likely to interfere with sleep. It’s not as strong for inflammation, but many people use it at night for pain relief without the sleep disruption. Some patients combine low-dose celecoxib in the morning with acetaminophen at night for balanced relief.
How long does it take for sleep to improve after stopping celecoxib?
If celecoxib was the main cause of sleep problems, many people notice improvement within 3-5 days of switching to another pain reliever or adjusting the timing. Full recovery of sleep quality can take up to 2 weeks, especially if chronic pain has disrupted your sleep cycle for months. Combining the change with good sleep habits speeds up recovery.
Are there natural alternatives to celecoxib that won’t hurt sleep?
Yes. Topical treatments like capsaicin cream or menthol gels can reduce joint pain without affecting sleep. Turmeric supplements (with black pepper for absorption) have mild anti-inflammatory effects and are generally sleep-friendly. Physical therapy, gentle yoga, and cognitive behavioral therapy for pain (CBT-P) also help reduce reliance on medication-and improve sleep naturally.



 Medications
Medications




Doug Pikul
October 31, 2025 AT 20:14Been on celecoxib for 3 years for knee arthritis. Took it at 8am like they said. Woke up at 3am every night like my joints were on fire. Switched to 100mg at bedtime and 100mg in the morning. Slept like a baby. No magic, just timing. Your body’s clock doesn’t care what the label says.
Craig Venn
November 2, 2025 AT 14:14Biggest oversight in most clinical guidance is treating pain and sleep as separate variables. COX-2 inhibition disrupts circadian prostaglandin flux which modulates SCN activity. Melatonin suppression is dose-dependent and circadian-phase sensitive. Nighttime dosing isn't anecdotal-it's pharmacokinetic optimization. Also, acetaminophen has zero COX-2 effect so it’s the ideal adjunct for nocturnal analgesia without sleep architecture disruption. Stop treating symptoms. Treat the system.
MaKayla VanMeter
November 2, 2025 AT 22:34OMG I KNEW IT 😭 I took celecoxib for 2 weeks and started having nightmares about my knees screaming. I thought I was going crazy. Then I read this and I cried. Like… literally cried. I’m switching to turmeric gummies now. No more big pharma lies 💪🌿
Sarah Major
November 4, 2025 AT 02:39People just don’t want to accept that their sleep problems are their own fault. You take a pill, then blame it for not sleeping. Try sleeping in a dark room. Turn off your phone. Maybe your brain is just lazy. Celecoxib isn’t the villain. Your habits are.
Nate Barker
November 5, 2025 AT 16:37This whole post is a shill for Big Pharma. Celecoxib doesn’t mess with sleep. It’s the stress of being broke and working two jobs. Also, you’re probably scrolling TikTok till 2am. Stop blaming drugs. Blame your life.
Alicia Buchter
November 6, 2025 AT 02:10How quaint. You all treat sleep like a commodity you can optimize with a pill schedule. Have you ever considered that chronic pain isn’t just a biological glitch-it’s a manifestation of existential dissonance? The body remembers trauma. The prostaglandins? Just the messenger. You want better sleep? Stop treating your pain like a math problem. Start listening. Really listening. To the silence. To the ache. To the part of you that’s been screaming since 2017.
I used to take celecoxib at night. Then I started journaling. Then I stopped taking it. Then I cried in the shower for three days straight. And then-I slept. Not because of timing. Not because of acetaminophen. But because I finally stopped fighting what my body was trying to tell me.
You can’t pharmacologically outmaneuver grief. Pain is just the echo.
Just saying.
anthony perry
November 7, 2025 AT 15:24Evening dose works. Done.
Christine Mae Raquid
November 7, 2025 AT 19:06so like… i tried taking it at night and i just felt weird like my brain was buzzing?? like not sleepiness but like… i dont know… electric?? and then i started dreaming about my knee being a robot?? idk man i think its the meds but also maybe the wifi??
Amber Walker
November 8, 2025 AT 14:10YESSSS this is so real!! I was SO tired all day even after 9 hours of sleep!! I thought I was just old!! But then I tried the nighttime dose and BAM!! I woke up feeling like a human again!! I’m telling all my friends!! You guys are gonna thank me later!!
Torrlow Lebleu
November 10, 2025 AT 00:34Everyone’s missing the point. Celecoxib doesn’t cause sleep issues. It’s the NSAID industry’s way of keeping you dependent. They know if you sleep better, you’ll stop taking their pills. That’s why they don’t tell you about melatonin suppression. They profit from your insomnia. Wake up.